Overview of Alcohol-Related Liver Disease
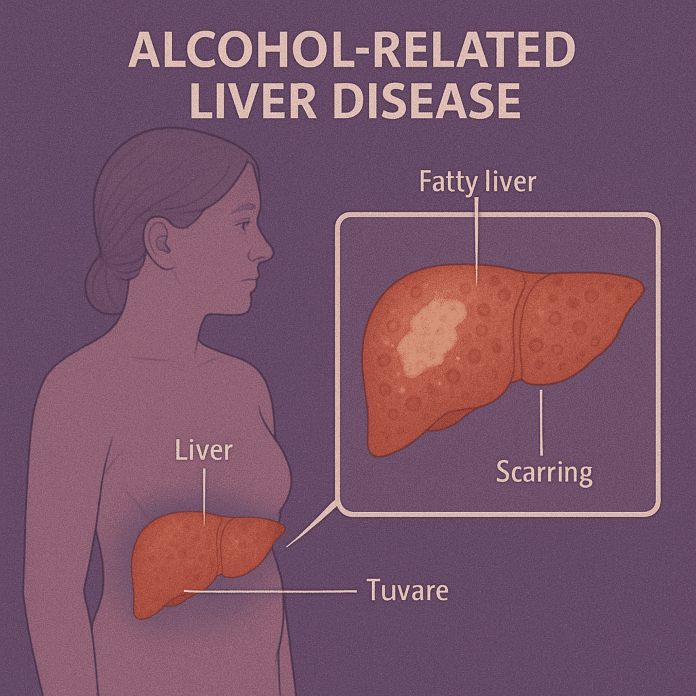
Alcohol-related liver disease (ARLD) is a progressive liver condition caused by excessive and prolonged alcohol consumption. The liver metabolizes alcohol, but chronic heavy drinking overwhelms its capacity, leading to inflammation, fat accumulation, scarring, and eventually liver failure.
ARLD develops in three main stages that may overlap:
- Alcoholic fatty liver disease (steatosis): Fat accumulates in liver cells; often reversible with abstinence.
- Alcoholic hepatitis: Inflammation and liver cell damage occur, leading to jaundice, fever, and liver dysfunction.
- Alcoholic cirrhosis: Irreversible scarring replaces healthy liver tissue, impairing liver function and increasing the risk of liver failure and liver cancer.
ARLD is a major global cause of chronic liver disease and death, but early diagnosis and complete cessation of alcohol can significantly improve outcomes and even reverse early-stage disease.
Commonly Associated with Alcohol-Related Liver Disease
ARLD is strongly associated with lifestyle and underlying health factors, including:
- Chronic heavy alcohol consumption: Typically over 20–30 g/day (about 2–3 drinks) in women and 40–50 g/day in men for several years.
- Binge drinking: Periodic heavy drinking can accelerate liver damage.
- Duration of alcohol use: Longer exposure increases risk.
- Genetic susceptibility: Variations in alcohol-metabolizing enzymes.
- Sex: Women are more susceptible to alcohol-related liver damage at lower consumption levels.
- Obesity and metabolic syndrome: Increase risk and accelerate disease progression.
- Coexisting viral hepatitis (e.g., hepatitis C).
- Poor nutrition: Often present in heavy drinkers and worsens liver injury.
Causes of Alcohol-Related Liver Disease
The primary cause of ARLD is chronic excessive alcohol intake. When the liver metabolizes alcohol, it produces toxic byproducts such as acetaldehyde and reactive oxygen species, which damage liver cells and trigger inflammation. Over time, repeated injury leads to fibrosis (scarring) and loss of liver function.
Pathophysiological processes include:
- Fat accumulation (steatosis): Alcohol alters fat metabolism, leading to triglyceride buildup in liver cells.
- Oxidative stress: Free radicals damage liver cell membranes and DNA.
- Inflammation: Cytokines and immune responses exacerbate liver injury.
- Fibrosis and cirrhosis: Chronic inflammation promotes scar tissue formation, replacing healthy tissue and disrupting liver architecture.
Symptoms of Alcohol-Related Liver Disease
ARLD is often asymptomatic in its early stages, particularly during fatty liver disease. Symptoms typically appear as the disease progresses to hepatitis or cirrhosis.
Early-stage (Fatty Liver):
- Often asymptomatic
- Fatigue
- Mild right upper abdominal discomfort
Alcoholic Hepatitis:
- Jaundice (yellowing of skin and eyes)
- Fever
- Nausea, vomiting, and abdominal pain
- Loss of appetite and weight loss
- Swollen, tender liver
- General weakness
Cirrhosis (Advanced Stage):
- Severe jaundice
- Fluid accumulation in the abdomen (ascites)
- Swelling of legs (edema)
- Easy bruising or bleeding
- Confusion and drowsiness (hepatic encephalopathy)
- Spider angiomas (small blood vessels on the skin)
- Gastrointestinal bleeding (due to esophageal varices)
Severe alcoholic hepatitis and cirrhosis can be life-threatening and require urgent medical attention.
Exams & Tests for Alcohol-Related Liver Disease
Diagnosis is based on medical history, physical examination, blood tests, and imaging. Key steps include:
- Medical history: Assessing alcohol intake and duration.
- Physical exam: Checking for jaundice, enlarged liver, ascites, or signs of chronic liver disease.
Laboratory Tests:
- Liver function tests (LFTs): Elevated AST, ALT (often AST > ALT), alkaline phosphatase, and bilirubin.
- Gamma-glutamyl transferase (GGT): Often elevated due to alcohol use.
- Complete blood count (CBC): May show anemia, leukocytosis, or thrombocytopenia.
- Coagulation tests: Elevated INR suggests advanced disease.
Imaging:
- Ultrasound, CT, or MRI: Assess liver size, fatty changes, nodularity, and ascites.
- Elastography (FibroScan): Measures liver stiffness to assess fibrosis and cirrhosis.
Liver biopsy:
- Confirms diagnosis and assesses disease severity if diagnosis remains uncertain.
Treatment of Alcohol-Related Liver Disease
The cornerstone of ARLD treatment is complete abstinence from alcohol, which can halt disease progression and even reverse early damage. Treatment strategies depend on disease stage and severity.
1. Lifestyle and Supportive Care:
- Alcohol cessation: The most important step; may require counseling, rehabilitation, or support groups.
- Nutritional therapy: High-protein, high-calorie diets with vitamin and mineral supplementation (especially thiamine).
- Vaccination: Against hepatitis A and B to prevent further liver damage.
2. Medical Management:
- Corticosteroids (e.g., prednisolone): For severe alcoholic hepatitis to reduce inflammation.
- Pentoxifylline: Sometimes used to prevent hepatorenal syndrome (limited evidence).
- Management of complications: Diuretics for ascites, lactulose for hepatic encephalopathy, and beta-blockers for variceal bleeding risk.
3. Advanced Therapies:
- Endoscopic or surgical interventions: For variceal bleeding or portal hypertension.
- Liver transplantation: Considered for end-stage cirrhosis or liver failure in patients who maintain alcohol abstinence.
Early intervention significantly improves prognosis. Patients with fatty liver often recover fully within weeks of stopping alcohol, whereas advanced cirrhosis has a 5-year survival rate of ~50%.
Source
- European Association for the Study of the Liver (EASL). “Clinical Practice Guidelines: Management of alcohol-related liver disease.” J Hepatol 2018; 69(1):154–181.
- Gao B, Bataller R. “Alcoholic liver disease: pathogenesis and new therapeutic targets.” Gastroenterology 2011; 141(5):1572–1585.
- National Institute for Health and Care Excellence (NICE). “Alcohol-related liver disease: diagnosis and management.” NICE Guideline NG50, 2016.