Overview of Arterial Thrombosis
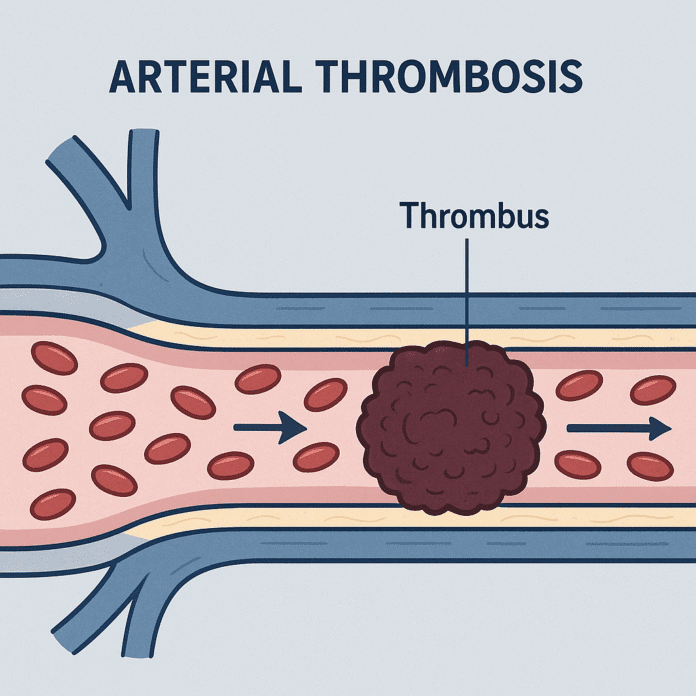
Arterial thrombosis is the formation of a blood clot (thrombus) inside an artery, obstructing blood flow to vital organs and tissues. Because arteries carry oxygen-rich blood from the heart to the body, a blockage can lead to serious, life-threatening conditions such as heart attack, stroke, or limb ischemia.
Arterial thrombosis usually develops on a background of atherosclerosis — the buildup of fatty plaques inside arteries — which can rupture and trigger clot formation. The condition often occurs suddenly and without warning, and immediate medical treatment is crucial to restore blood flow and prevent permanent tissue damage.
Commonly Associated With Arterial Thrombosis
Several conditions and risk factors significantly increase the likelihood of arterial thrombosis:
- Atherosclerosis – the most common underlying cause.
- Coronary artery disease (CAD) – leading to myocardial infarction (heart attack).
- Cerebrovascular disease – leading to ischemic stroke.
- Peripheral arterial disease (PAD) – leading to acute limb ischemia.
- Hypertension – damages arterial walls.
- Hyperlipidemia – increases plaque formation.
- Diabetes mellitus – accelerates atherosclerosis and endothelial damage.
- Smoking – promotes vascular injury and platelet activation.
- Atrial fibrillation (less common for arterial, but may cause embolic stroke).
- Obesity and sedentary lifestyle.
- Family history of cardiovascular disease.
Causes of Arterial Thrombosis
Arterial thrombosis is primarily caused by rupture or erosion of an atherosclerotic plaque, which exposes underlying tissue and triggers the coagulation cascade. This leads to platelet activation, aggregation, and thrombus formation.
Major causes include:
- Atherosclerotic plaque rupture: The fibrous cap of a plaque breaks open, exposing pro-thrombotic material and causing clot formation.
- Endothelial injury: High blood pressure, smoking, and diabetes damage the vessel lining, increasing thrombosis risk.
- Turbulent blood flow: Can occur at arterial branch points or in aneurysms, promoting clot formation.
- Hypercoagulable states: Rare genetic or acquired clotting disorders.
- Post-surgical or traumatic vascular injury: Can trigger local thrombosis.
Symptoms of Arterial Thrombosis
Symptoms vary depending on which artery is affected and how quickly the blockage develops. They often occur suddenly and require emergency attention.
Coronary artery thrombosis (Heart attack):
- Severe chest pain or pressure (angina)
- Pain radiating to arm, jaw, or back
- Shortness of breath
- Nausea or vomiting
- Sweating and lightheadedness
Cerebral artery thrombosis (Ischemic stroke):
- Sudden weakness or numbness, especially on one side
- Difficulty speaking or understanding speech
- Vision problems
- Severe headache
- Loss of coordination or balance
Peripheral arterial thrombosis (Limb ischemia):
- Sudden, severe limb pain
- Cold, pale, or blue limb
- Numbness or paralysis
- Loss of pulse in the affected area
Untreated arterial thrombosis can lead to permanent tissue damage, organ failure, or death.
Exams & Tests for Arterial Thrombosis
Diagnosis depends on the affected artery and often requires urgent evaluation.
- Medical history and physical examination: Assess risk factors and symptoms.
- Blood tests:
- Cardiac enzymes (e.g., troponin) – elevated in myocardial infarction.
- Coagulation profile – to check for clotting abnormalities.
- Electrocardiogram (ECG): Detects heart attack or ischemia.
- Imaging:
- Angiography: Gold standard for visualizing arterial blockages.
- CT or MR angiography: Detects thrombi in brain or peripheral arteries.
- Duplex ultrasound: For limb or carotid artery thrombosis.
- Brain imaging (CT/MRI): Essential in suspected stroke to distinguish ischemic from hemorrhagic causes.
Treatment of Arterial Thrombosis
Treatment aims to restore blood flow quickly, prevent further clot formation, and reduce the risk of recurrence. The approach depends on the site and severity of the thrombosis.
1. Immediate Emergency Treatment:
- Antiplatelet drugs: Aspirin or clopidogrel to prevent further clot growth.
- Anticoagulants: Heparin or warfarin to prevent new clots.
- Thrombolysis: Intravenous “clot-busting” drugs (e.g., alteplase) for stroke or myocardial infarction, ideally within a few hours of symptom onset.
2. Interventional and Surgical Procedures:
- Percutaneous coronary intervention (PCI): Balloon angioplasty and stent placement to reopen blocked coronary arteries.
- Thrombectomy: Surgical removal of the clot in severe cases or when thrombolysis is contraindicated.
- Endarterectomy: Surgical removal of plaque from arteries, often used in carotid artery disease.
3. Long-Term Management:
- Antiplatelet therapy: Lifelong aspirin or dual antiplatelet therapy for secondary prevention.
- Statins: To lower cholesterol and stabilize plaques.
- Blood pressure and diabetes control: Through lifestyle changes and medication.
- Smoking cessation and lifestyle modification: Critical to prevent recurrence.
Source
- Capodanno D, et al. “Antithrombotic therapy for arterial thrombosis.” Nat Rev Cardiol 2020; 17(9):543–558.
- Libby P, et al. “Mechanisms of acute coronary syndromes and their implications for therapy.” N Engl J Med 2019; 380(23):2219–2231.
- Powers WJ, et al. “Guidelines for the early management of acute ischemic stroke.” Stroke 2018; 49(3):e46–e110.