Overview of Bile Duct Cancer (Cholangiocarcinoma)
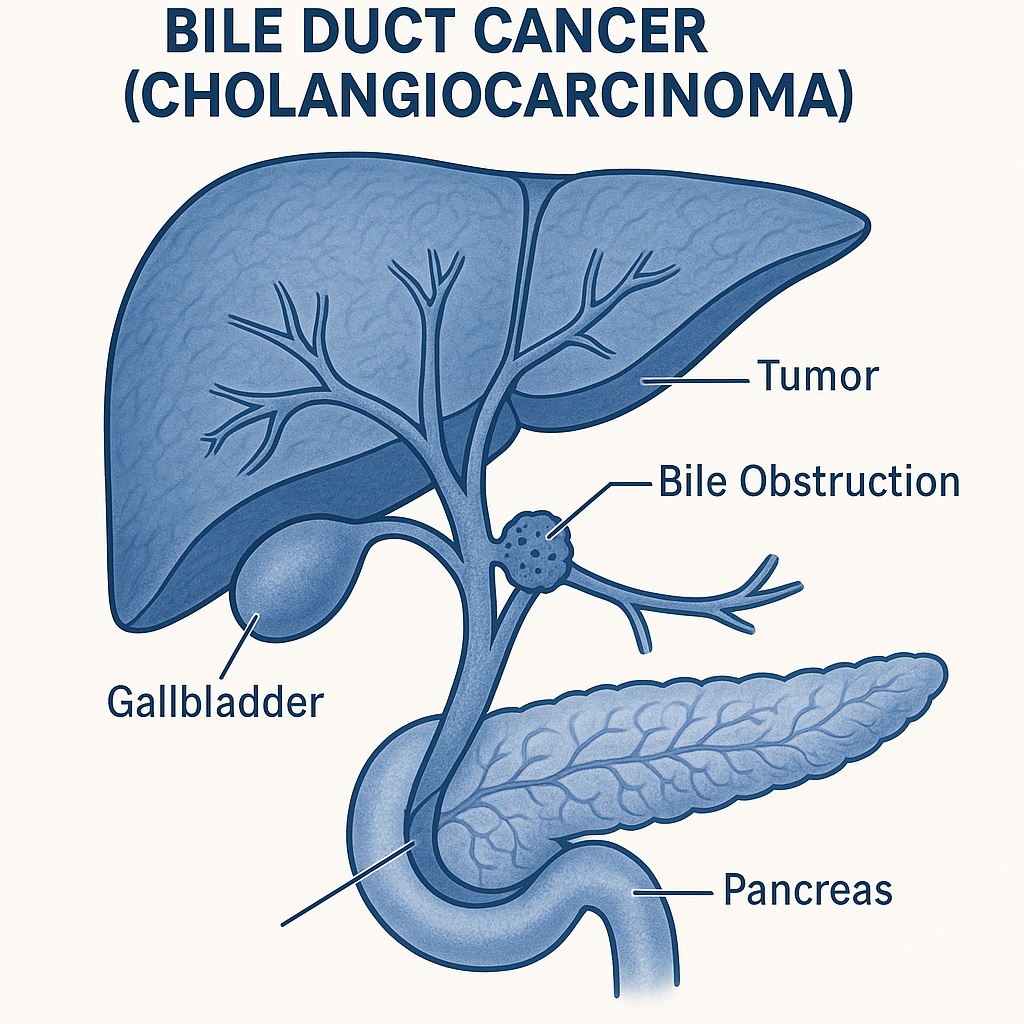
Bile duct cancer, medically known as cholangiocarcinoma, is a rare and aggressive cancer that arises from the epithelial cells lining the bile ducts, which transport bile from the liver to the gallbladder and small intestine. It can develop inside the liver (intrahepatic), outside the liver (extrahepatic), or at the junction where the right and left hepatic ducts meet (perihilar, also called Klatskin tumor).
Cholangiocarcinoma often develops slowly over many years, and symptoms usually appear only when the disease is advanced, making early diagnosis difficult. It accounts for about 3% of all gastrointestinal cancers, but its incidence is rising worldwide. Early detection, when possible, significantly improves treatment outcomes.
Commonly Associated With Bile Duct Cancer
Several risk factors and conditions are linked with an increased risk of cholangiocarcinoma:
- Primary sclerosing cholangitis (PSC): Chronic inflammation and scarring of bile ducts.
- Chronic biliary infections or inflammation: Recurrent cholangitis, hepatolithiasis.
- Congenital bile duct anomalies: Choledochal cysts, Caroli disease.
- Parasitic infections: Opisthorchis viverrini and Clonorchis sinensis (common in Southeast Asia).
- Chronic liver disease: Hepatitis B or C infection, cirrhosis, nonalcoholic steatohepatitis (NASH).
- Exposure to certain chemicals: Thorotrast (historical contrast agent), dioxins.
- Age: Most cases occur in people over 50 years old.
- Diabetes and obesity: Associated with increased risk of intrahepatic cholangiocarcinoma.
Causes of Bile Duct Cancer
The exact cause of cholangiocarcinoma is not always known, but most cases are linked to chronic inflammation and injury to the bile duct lining, which lead to DNA damage and uncontrolled cell growth.
Key mechanisms include:
- Chronic inflammation: Persistent irritation causes repeated cell turnover, increasing mutation risk.
- Bile stasis: Prolonged obstruction of bile flow contributes to cellular damage and malignant transformation.
- Genetic mutations: Alterations in genes such as IDH1/2, FGFR2, KRAS, TP53, and BAP1 are implicated.
- Environmental and infectious exposures: Parasitic infections and certain toxins can directly damage bile duct epithelium.
Symptoms of Bile Duct Cancer
Cholangiocarcinoma often remains asymptomatic in early stages. Symptoms typically develop once bile flow is obstructed or the disease has progressed.
Common signs and symptoms include:
- Jaundice (yellowing of skin and eyes): Caused by bile flow obstruction.
- Itchy skin (pruritus): Due to bile salt accumulation.
- Dark urine and pale stools: Results from impaired bile drainage.
- Abdominal pain: Often dull and located in the upper right quadrant.
- Unexplained weight loss and loss of appetite.
- Fever and chills: May occur with secondary infection (cholangitis).
- Fatigue and general weakness.
In advanced stages, symptoms such as abdominal swelling (ascites), hepatomegaly, and liver failure may occur.
Exams & Tests for Bile Duct Cancer
Diagnosis involves a combination of blood tests, imaging, and biopsy to confirm malignancy and determine the tumor’s location and extent.
- Blood tests:
- Liver function tests (LFTs): Elevated bilirubin, alkaline phosphatase, and gamma-GT.
- Tumor markers: Elevated CA 19-9 and CEA may support diagnosis but are not specific.
- Imaging studies:
- Ultrasound: Initial evaluation for bile duct dilation and obstruction.
- CT scan or MRI: Detailed imaging of the tumor and surrounding structures.
- Magnetic resonance cholangiopancreatography (MRCP): Non-invasive visualization of bile ducts.
- Endoscopic retrograde cholangiopancreatography (ERCP): Allows imaging, bile duct sampling, and stent placement.
- Percutaneous transhepatic cholangiography (PTC): Alternative imaging for bile ducts.
- Biopsy and histopathology:
- Obtained via ERCP, percutaneous needle biopsy, or surgical exploration to confirm malignancy.
- Staging:
- TNM classification (Tumor size, Node involvement, Metastasis) determines treatment approach and prognosis.
Treatment of Bile Duct Cancer
Treatment depends on the tumor’s location, size, stage, and whether it has spread, as well as the patient’s overall health.
1. Surgical Treatment (Potentially Curative):
- Resection: Surgical removal of the tumor and surrounding tissue.
- Liver resection or transplantation: For intrahepatic or perihilar cholangiocarcinoma if localized.
- Bile duct reconstruction: May be required after tumor removal.
2. Non-Surgical Treatments:
- Biliary drainage or stenting: To relieve obstruction and reduce jaundice.
- Photodynamic therapy (PDT): Light-based treatment to destroy cancer cells and improve bile flow.
- Radiofrequency ablation (RFA): Minimally invasive option for local tumor control.
3. Systemic Therapy:
- Chemotherapy: Combination regimens such as gemcitabine and cisplatin are standard for advanced disease.
- Targeted therapy: FGFR inhibitors (e.g., pemigatinib) or IDH1 inhibitors (e.g., ivosidenib) for specific mutations.
- Immunotherapy: PD-1 inhibitors (e.g., pembrolizumab) for tumors with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR).
4. Palliative Care:
- Focuses on symptom relief and improving quality of life in advanced or inoperable cases.
Prognosis:
- Prognosis depends on stage and resectability. Early-stage resected tumors have a 5-year survival rate of 20–40%, but advanced disease has a poor prognosis with median survival under 12 months.
Source
- Valle JW, et al. “Biliary tract cancer.” Lancet 2021; 397(10272):428–444.
- Bridgewater J, et al. “Guidelines for the diagnosis and management of cholangiocarcinoma.” Gut 2020; 69(8):1352–1373.
- Rizvi S, Gores GJ. “Pathogenesis, diagnosis, and management of cholangiocarcinoma.” Gastroenterology 2022; 162(6):1592–1611.