Overview Of Genital Warts (Human Papillomavirus)
Genital warts (human papillomavirus) are a common sexually transmitted infection. They are passed on through anal, vaginal, and, rarely, oral sex. Treatment from a sexual health clinic can help Genital warts go away.
Genital warts are small, raised, usually painless growths. They are caused by the human papillomavirus (HPV) which can be passed on through sex without a condom. There are over 100 different strains of HPV. The strain of HPV that causes genital warts is different from the strain that causes genital cancers, such as cervical cancer. The HPV that causes warts isn’t linked to cancer and doesn’t cause any more serious health problems. Warts themselves can be treated and will clear.
Commonly Associated With
Condylomata acuminata; Penile warts; Human papillomavirus (HPV); Venereal warts; Condyloma; HPV DNA test; Sexually transmitted disease (STD) – warts; Sexually transmitted infection (STI) – warts; LSIL-HPV; Low-grade dysplasia-HPV; HSIL-HPV; High-grade dysplasia HPV; HPV; Cervical cancer – genital warts
Causes Of Genital Warts (Human Papillomavirus)
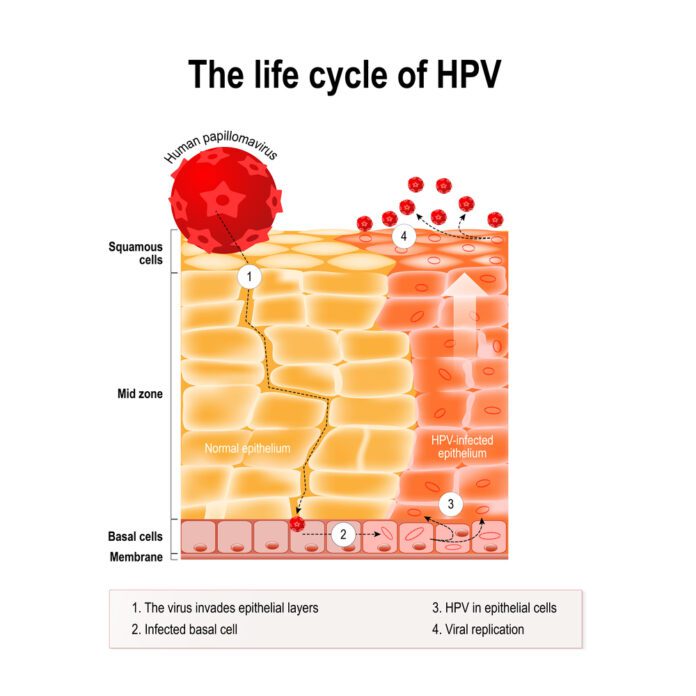
The virus that causes genital warts is called human papillomavirus (HPV). HPV infection is the most common sexually transmitted infection (STI). There are more than 180 types of HPV. Many cause no problems. Some cause warts on other parts of the body and not the genitals. Types 6 and 11 are most commonly linked to genital warts.
Certain other types of HPV can lead to precancerous changes in the cervix, or to cervical cancer. These are called high-risk types of HPV. They can also lead to vaginal or vulvar cancer, anal cancer, and throat or mouth cancer.
Important facts about HPV:
• HPV infection spreads from one person to another through sexual contact involving the anus, mouth, or vagina. The virus can be spread, even if you DO NOT see warts.
• You may not see warts for 6 weeks to 6 months after becoming infected. You may not notice them for years.
• Not everyone who has come into contact with the HPV virus and genital warts will develop them.
You are more likely to get genital warts and spread them more quickly if you:
• Have multiple sexual partners
• Are sexually active at an early age
• Use tobacco or alcohol
• Have a viral infection, such as herpes, and are stressed at the same time
• Are pregnant
• Have a weakened immune system due to a condition such as diabetes, pregnancy, HIV/AIDS, or medicines
If a child has genital warts, sexual abuse should be suspected as a possible cause.
Symptoms Of Genital Warts (Human Papillomavirus)
Genital warts can appear as a single wart or as multiple warts in a cluster.
Symptoms include:
● one or more small, flesh-colored, or grey painless growths or lumps around the vagina, penis, anus, or upper thighs
● itching or bleeding from genitals or anus
● a change to the normal flow of pee (for example, sideways), that doesn’t go away.
Be aware that warts may be difficult to notice if they are internal (inside the vagina or anus) and that many people with the strain of HPV that causes genital warts will not develop any symptoms or know that they have it.
Symptoms of genital warts can appear weeks, months, or years after you were in contact with the virus that causes them.
If you have symptoms of genital warts it’s important to visit a health clinic to have them checked.
Treatment Of Genital Warts (Human Papillomavirus)
The sooner genital warts are treated, the easier they are to get rid of. There are two main types of treatment for genital warts. The type of treatment you receive will depend on the type of warts you have and where the warts are.
Treatments include:
● applying a cream, lotion, or chemicals to warts
● destroying warts by freezing, heating, or removing them.
It may take several weeks for the treatment to work. During this time, it may be advised to avoid soaps or creams and lotions that could irritate the skin. You might also be advised not to have sex until you or partner have finished the treatment, and warts have gone.
Although these treatments can remove warts themselves, there’s no cure for the virus that causes warts. Some people’s bodies, however, can clear the virus over time.
You should always check with a healthcare worker before using treatments for genital warts. Many wart treatments are designed to be used on hands and feet and should not be used on the genitals.
Genital warts and pregnancy
Pregnant women can pass genital warts on to their babies during childbirth, but this is rare. Talk to the healthcare worker if you are pregnant and think you might have genital warts. They will be able to advise you which treatment to use, as not all of the treatments available are suitable for pregnant women.
Genital warts, HIV and sexual health
If you have genital warts you should also test for HIV and other STIs. Having an STI, including genital warts, can increase the risk of getting HIV. This is because having an STI makes it easier for HIV to get into the body and cause an infection.
People living with HIV can also be more likely to get genital warts or have more severe cases of genital warts. This is especially the case for people who aren’t on treatment or who have a lower CD4 count. You’re more vulnerable to infections, like genital warts, if the immune system is weaker.
Speak to the healthcare provider if you are living with HIV and taking treatment for genital warts, to make sure that the medication won’t affect the antiretroviral treatment (ART).
(A CD4 count is a blood test to check the amount of CD4 cells in the body. CD4 cells are a type of white blood cell (WBC). They play a key role in the immune system. They alert other immune cells to the presence of infections such as bacteria and other viruses in the body. CD4 cells are also a subset of immune cells called T cells.
When a person is living with HIV, the virus attacks the CD4 cells in their blood. This process damages CD4 cells and causes the number of them in the body to drop, making it difficult to fight infections.
CD4 counts show the robustness of the immune system. A healthy immune system normally has a CD4 count ranging from 500 to 1,600 cells per cubic millimeter of blood (cells/mm3).
When a CD4 count is lower than 200 cell/mm3, a person will receive a diagnosis of AIDS. AIDS occurs in stage 3 of HIV. At this stage, the body’s immune system is weak due to the low number of CD4 cells available to fight disease.)
Other
How do you get genital warts?
Genital warts can be passed on through vaginal or anal sex without a condom and by sharing sex toys. The virus is transmitted through close genital contact, which means that you can get and pass on warts if you touch genitals with someone, even if you don’t have penetrative sex or ejaculate (cum).
Although it’s rare, genital warts can also be passed on through oral sex and affect the mouth and throat.
You can only get genital warts from someone else who has the virus but be aware that not everyone will know if they have it. If the warts are internal someone may not notice them and people can pass on the virus even if they don’t have any symptoms.
You can’t get genital warts from kissing, hugging, swimming pools, sharing towels, or cutlery.
If a woman has genital warts while pregnant, there is a risk that she could pass them on to her baby at birth. This isn’t very common, but pregnant women must seek advice from a healthcare worker if they notice any symptoms.
Prevention
The best way to prevent genital warts is to use a condom for vaginal, anal, and oral sex. If you’re sharing sex toys these should be covered with a new condom for each partner and washed between use.
If you have symptoms that could be genital warts you should go to a health clinic to have these checked. If you have genital warts, you may be advised to avoid sex while they’re being treated. If you do have sex, make sure that the warts are covered with a condom. This area of skin should be covered with a condom even after warts have gone. You can still pass the virus on for up to three months after warts have disappeared. Avoid rubbing or touching warts, in case you spread the infection to the surrounding area. If you find out that you have genital warts the partner should also get checked.
Talking about sexual health with partners, and letting each other know about any symptoms or infections, will help you decide how to have safer sex together.
Reducing the number of sexual partners can also help you reduce the risk of getting sexually transmitted infections, like genital warts. If you are having sex with multiple partners, it’s even more important to use condoms and to have regular STI tests.
Condoms are the best form of protection against STIs and pregnancy. Other contraceptives including the contraceptive pill will not prevent genital warts, neither will PrEP.
PRE-EXPOSURE PROPHYLAXIS (PREP)
Pre-exposure prophylaxis (PrEP) is a course of HIV drugs taken by HIV-negative people to prevent infection.
Taking PrEP correctly will virtually eliminate the risk of getting HIV.
PrEP won’t protect against other sexually transmitted infections (STIs) such as hepatitis C. Condoms are still the best protection from these STIs.
PrEP is not taken for life – it is only taken for short periods when a person may be at risk of HIV infection.
Vaccine
The HPV vaccine, developed to protect against more serious forms of HPV, can also prevent genital warts. The vaccine does not guarantee that you will not develop genital warts in the future, but it will reduce the risk. It’s best to have the vaccine before you start having sex.
Ask a healthcare worker to find out if you can get the HPV vaccine where you are.
Medical Examination
Healthcare professionals will usually diagnose warts by looking at them. They may check for hidden warts, by looking inside the vagina and or anus. If you have a problem urinating, a specialist may look at the urethra (the tube that carries pee from the bladder).
This examination shouldn’t be painful and you are welcome to have someone with you for the appointment if it would make you feel more comfortable. It’s not something that you should feel embarrassed about, remember that the healthcare professional will do this all the time.
Source