Uses
Clomipramine is used to treat people with obsessive-compulsive disorder (a condition that causes repeated unwanted thoughts and the need to perform certain behaviors over and over). Clomipramine is in a group of medications called tricyclic antidepressants. It works by increasing the amount of serotonin, a natural substance in the brain that is needed to maintain mental balance.
Side Effects Of Clomipramine
Clomipramine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dry mouth
- nausea
- vomiting
- diarrhea
- constipation
- nervousness
- decreased sexual ability
- decreased memory or concentration
- headache
- stuffy nose
- change in appetite or weight
Some side effects of clomipramine may be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING or SPECIAL PRECAUTIONS sections, call your doctor immediately or get emergency medical treatment:
- uncontrollable shaking of a part of the body
- seizures
- fast, irregular, or pounding heartbeat
- difficulty urinating or loss of bladder control
- believing things that are not true
- hallucinations (seeing things or hearing voices that do not exist)
- shakiness
- difficulty breathing or fast breathing
- severe muscle stiffness
- unusual tiredness or weakness
- sore throat, fever, and other signs of infection
Warnings & Precautions
Before taking clomipramine:
- tell your doctor and pharmacist if you are allergic to clomipramine, other tricyclic antidepressants such as amitriptyline (Elavil), amoxapine (Asendin), desipramine (Norpramin), doxepin (Adapin, Sinequan), imipramine (Tofranil), nortriptyline (Aventyl, Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil); any other medications, or any of the inactive ingredients in clomipramine capsules. Ask your doctor or pharmacist for a list of the inactive ingredients.
- tell your doctor if you are taking a monoamine oxidase (MAO) inhibitor such as isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate), or if you have stopped taking an MAO inhibitor within the past 14 days. Your doctor will probably tell you not to take clomipramine. If you stop taking clomipramine, you should wait at least 14 days before you start to take an MAO inhibitor.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take with clomipramine. Be sure to mention any of the following: anticoagulants (‘blood thinners’) such as warfarin (Coumadin, Jantoven); benztropine (Cogentin); cimetidine (Tagamet); clonidine (Catapres); dicyclomine (Bentyl); digoxin (Lanoxin); disulfiram; flecainide (Tambocor); guanethidine (Ismelin); haloperidol (Haldol); levodopa (Sinemet, Dopar); medications for nausea, dizziness, or mental illness; methylphenidate (Concerta, Metadate, Ritalin); oral contraceptives; phenobarbital; phenytoin; propafenone (Rythmol); quinidine; secobarbital (Seconal); sedatives; selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac, Sarafem), sertraline (Zoloft), and paroxetine (Paxil); tranquilizers; and trihexyphenidyl (Artane); and vitamins. Your doctor may need to change the doses of your medication or monitor you more carefully for side effects. Your doctor may tell you not to take clomipramine if you have stopped taking fluoxetine during the past 5 weeks.
- tell your doctor if you have recently had a heart attack. Your doctor may tell you that you should not take clomipramine.
- tell your doctor if you are being treated with electroshock therapy (a procedure in which small electric shocks are administered to the brain to treat certain mental illnesses) if you drink or have ever drunk large amounts of alcohol, and if you have or have ever had seizures, brain damage, problems with your urinary system or prostate (a male reproductive organ), irregular heartbeat, problems with your blood pressure, thyroid problems, or heart, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking clomipramine, call your doctor.
- talk to your doctor about the risks and benefits of taking clomipramine if you are 65 years of age or older. Older adults should not usually take clomipramine because it is not as safe or effective as other medications that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking clomipramine.
- you should know that this medication may make you drowsy and may increase the risk that you will have a seizure. Do not drive a car, operate machinery, swim, or climb until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- tell your doctor if you use tobacco products. Cigarette smoking may decrease the effectiveness of this medication.
- you should know that clomipramine may cause angle-closure glaucoma (a condition where the fluid is suddenly blocked and unable to flow out of the eye causing a quick, severe increase in eye pressure which may lead to a loss of vision). Talk to your doctor about having an eye examination before you start taking this medication. If you have nausea, eye pain, changes in vision, such as seeing colored rings around lights, and swelling or redness in or around the eye, call your doctor or get emergency medical treatment right away.
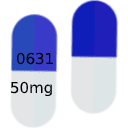
Clomipramine Dosage
Clomipramine comes as a capsule to take by mouth. At the beginning of treatment, clomipramine is usually taken three times a day with meals as the body adjusts to the medication. After several weeks of treatment, clomipramine is usually taken once a day at bedtime. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take clomipramine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may start you on a low dose of clomipramine and gradually increase your dose.
It may take several weeks or longer for you to feel the full benefit of clomipramine. Continue to take clomipramine even if you feel well. Do not stop taking clomipramine without talking to your doctor. If you suddenly stop taking clomipramine, you may experience withdrawal symptoms such as dizziness, nausea, vomiting, headache, weakness, sleep problems, fever, and irritability. Your doctor probably will decrease your dose gradually.
Other
Keep all appointments with your doctor.
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription of clomipramine.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.