Uses
Nebivolol is used alone or in combination with other medications to treat high blood pressure. Nebivolol is in a class of medications called beta-blockers. It works by relaxing blood vessels and slowing heart rate to improve blood flow and decrease blood pressure.
High blood pressure is a common condition and when not treated, can cause damage to the brain, heart, blood vessels, kidneys, and other parts of the body. Damage to these organs may cause heart disease, a heart attack, heart failure, stroke, kidney failure, loss of vision, and other problems. In addition to taking medication, making lifestyle changes will also help to control your blood pressure. These changes include eating a diet that is low in fat and salt, maintaining a healthy weight, exercising at least 30 minutes most days, not smoking, and using alcohol in moderation.
Side Effects Of Nebivolol
Nebivolol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- headache
- tiredness
- weakness
- dizziness
- diarrhea
- nausea
- stomach pain
- difficulty falling asleep or staying asleep
- numbness, burning or tingling in the hands, arms, feet, or legs
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
- chest pain
- slow heart rate
- difficulty breathing
- unusual weight gain
- rash
- swelling of the hands, feet, ankles, or lower legs
Nebivolol may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Warnings & Precautions
Before taking nebivolol:
- tell your doctor and pharmacist if you are allergic to nebivolol, any other medications, or any of the ingredients in nebivolol tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take with nebivolol. Be sure to mention any of the following: amiodarone (Cordarone, Pacerone); beta blockers such as acebutolol (Sectral), atenolol (Tenormin, in Tenoretic), betaxolol, bisoprolol (Zebeta, in Ziac), carvedilol (Coreg), labetalol, metoprolol (Lopressor, Toprol XL), nadolol (Corgard, in Corzide), pindolol, propranolol (Inderal, InnoPran XL, in Inderide), sotalol (Betapace, Betapace AF, Sorine), timolol; bupropion (Aplenzin, Forfivo XL, Wellbutrin, Zyban); calcium channel blockers such as diltiazem (Cardizem, Dilacor, others) and verapamil (Calan, Covera, Isoptin, Verelan, in Tarka); chlorpheniramine (antihistamine in allergy and cold medications); cimetidine; clomipramine (Anafranil); clonidine (Catapres, Kapvay, in Clorpres); digoxin (Lanoxin); disopyramide (Norpace); duloxetine (Cymbalta); fluoxetine (Prozac, Sarafem, Selfemra, in Symbyax); haloperidol (Haldol); insulin; oral medications for diabetes; methadone (Dolophine, Methadose); paroxetine (Paxil); propafenone (Rythmol); quinidine; reserpine; ritonavir (Norvir, in Kaletra); and sildenafil (Revatio, Viagra). Your doctor may need to change the doses of your medications or monitor you carefully for side effects while taking nebivolol.
- tell your doctor if you have a slow heart rate, heart or liver disease, or heart failure. Your doctor may tell you not to take nebivolol.
- tell your doctor if you have or have ever had asthma or other lung diseases, diabetes, hyperthyroidism (an overactive thyroid gland), problems with blood circulation, kidney disease, severe allergies, or pheochromocytoma (a tumor that develops on a gland near the kidneys and may cause high blood pressure and fast heart rate).
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking nebivolol, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking nebivolol.
- you should know that nebivolol may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that if you have allergic reactions to different substances, your reactions may be worse while you are using nebivolol, and your allergic reactions may not respond to the usual doses of injectable epinephrine.
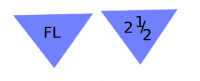
Nebivolol Dosage
Nebivolol comes as a tablet to take by mouth. It is usually taken with or without food once a day. To help you remember to take nebivolol, take it around the same time every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take nebivolol exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may start you on a low dose of nebivolol and gradually increase your dose not more than once every 2 weeks.
Nebivolol controls high blood pressure but does not cure it. It may take 2 weeks before the full benefit of nebivolol is seen in blood pressure readings. Continue to take nebivolol even if you feel well. Do not stop taking nebivolol without talking to your doctor. If you suddenly stop taking nebivolol it may cause angina (chest pain), heart attack, or irregular heartbeat. Your doctor will probably decrease your dose gradually over 1 to 2 weeks.
Other
Keep all appointments with your doctor. Your blood pressure should be checked regularly to determine your response to nebivolol. Your doctor may ask you to check your pulse (heart rate). Ask your pharmacist or doctor to teach you how to take your pulse. If your pulse is faster or slower than it should be, call your doctor.
Before having any laboratory test, tell your doctor and the laboratory personnel that you are taking nebivolol.
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.