Overview Of Systemic Lupus Erythematosus
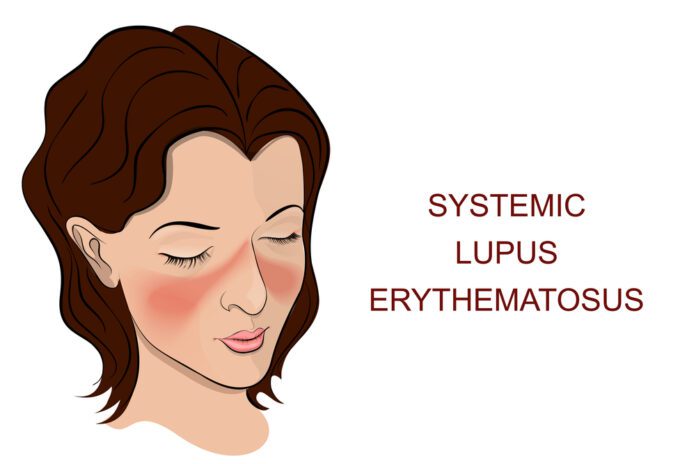
Systemic Lupus Erythematosus (SLE) is an autoimmune disease. In this disease, the immune system of the body mistakenly attacks healthy tissue. It can affect the skin, joints, kidneys, brain, and other organs.
Commonly Associated With
Disseminated lupus erythematosus; SLE; Lupus; Lupus erythematosus; Butterfly rash – SLE; Discoid lupus
Causes Of Systemic Lupus Erythematosus
The cause of SLE is not clearly known. It may be linked to the following factors:
- Genetic
- Environmental
- Hormonal
- Certain medicines
SLE is more common in women than men by nearly 10 to 1. It may occur at any age. However, it appears most often in young women between the ages of 15 and 44. In the US, the disease is more common in African Americans, Asian Americans, African Caribbeans, and Hispanic Americans.
Symptoms Of Systemic Lupus Erythematosus
Symptoms vary from person to person and may come and go. Everyone with SLE has joint pain and swelling at some time. Some develop arthritis. SLE often affects the joints of the fingers, hands, wrists, and knees.
Other common symptoms include:
- Chest pain when taking a deep breath.
- Fatigue.
- Fever with no other cause.
- General discomfort, uneasiness, or ill feeling (malaise).
- Hair loss.
- Weight loss.
- Mouth sores.
- Sensitivity to sunlight.
- Skin rash — A “butterfly” rash develops in about half the people with SLE. The rash is mostly seen over the cheeks and bridge of the nose. It can be widespread. It gets worse in sunlight.
- Swollen lymph nodes.
Other symptoms and signs depend on which part of the body is affected:
- Brain and nervous system — Headaches, weakness, numbness, tingling, seizures, vision problems, memory and personality changes
- Digestive tract — Abdominal pain, nausea, and vomiting
- Heart — Valve problems, inflammation of heart muscle or heart lining (pericardium)
- Lung — Buildup of fluid in the pleural space, difficulty breathing, coughing up blood
- Skin — Sores in the mouth
- Kidney — Swelling in the legs
- Circulation — Clots in veins or arteries, inflammation of blood vessels, constriction of blood vessels in response to cold (Raynaud phenomenon)
- Blood abnormalities including anemia, low white blood cell or platelet count
- Some people have only skin symptoms. This is called discoid lupus.
Exams & Tests
To be diagnosed with lupus, you must have 4 out of 11 common signs of the disease. Nearly all people with lupus have a positive test for antinuclear antibody (ANA). However, having a positive ANA alone does not mean you have lupus.
The health care provider will do a complete physical exam. You may have a rash, arthritis, or edema in the ankles. There may be an abnormal sound called a heart friction rub or pleural friction rub. Your provider will also do a nervous system exam.
Tests used to diagnose SLE may include:
- Antinuclear antibody (ANA)
- CBC with differential
- Chest x-ray
- Serum creatinine
- Urinalysis
You may also have other tests to learn more about your condition. Some of these are:
- Antinuclear antibody (ANA) panel
- Complement components (C3 and C4)
- Antibodies to double-stranded DNA
- Coombs test — direct
- Cryoglobulins
- ESR and CRP
- Kidney function blood tests
- Liver function blood tests
- Rheumatoid factor
- Antiphospholipid antibodies and lupus anticoagulant test
- Kidney biopsy
- Imaging tests of the heart, brain, lungs, joints, muscles, or intestines
Treatment Of Systemic Lupus Erythematosus
There is no cure for SLE. The goal of treatment is to control symptoms. Severe symptoms that involve the heart, lungs, kidneys, and other organs often need treatment by specialists.
Each person with SLE needs evaluation regarding:
- How active the disease is
- What part of the body is affected
- What form of treatment is needed
Mild forms of the disease may be treated with:
- NSAIDs for joint symptoms and pleurisy. Talk to your provider before taking these medicines.
- Low doses of corticosteroids, such as prednisone, for skin and arthritis symptoms.
- Corticosteroid creams for skin rashes.
- Hydroxychloroquine, a medicine also used to treat malaria.
- Methotrexate may be used to reduce the dose of corticosteroids
- Belimumab, a biologic medicine, may be helpful in some people.
Treatments for more severe SLE may include:
- High-dose corticosteroids.
- Immunosuppressive medicines (these medicines suppress the immune system). These medicines are used if you have severe lupus that is affecting the nervous system, kidney, or other organs. They may also be used if you do not get better with corticosteroids, or if your symptoms get worse when you stop taking corticosteroids.
- Medicines most commonly used include mycophenolate, azathioprine, and cyclophosphamide. Because of its toxicity, cyclophosphamide is limited to a short course of 3 to 6 months. Rituximab (Rituxan) is used in some cases as well.
- Blood thinners, such as warfarin (Coumadin), for clotting disorders such as antiphospholipid syndrome.
If you have SLE, it is also important to:
- Wear protective clothing, sunglasses, and sunscreen when in the sun.
- Get preventive heart care.
- Stay up-to-date with immunizations.
- Have tests to screen for thinning of the bones (osteoporosis).
- Avoid tobacco and drink minimal amounts of alcohol.