Overview of Acute Myeloid Leukaemia
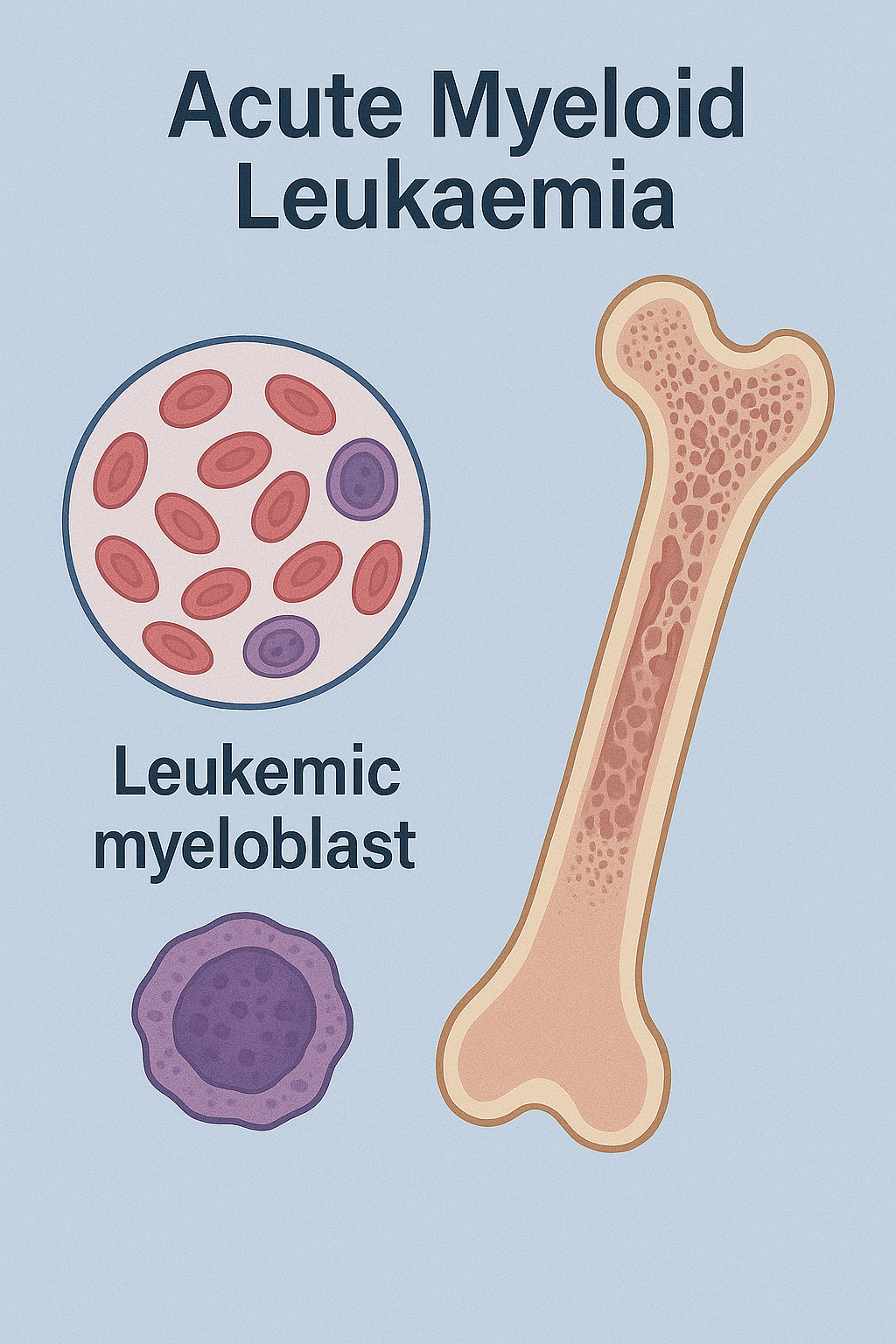
Acute myeloid leukaemia (AML) is a fast-growing cancer of the blood and bone marrow characterized by the uncontrolled proliferation of immature myeloid cells, called myeloblasts. These abnormal cells accumulate in the bone marrow and bloodstream, interfering with the production of normal red blood cells, white blood cells, and platelets. AML can progress rapidly and requires prompt diagnosis and treatment.
Although AML is most common in adults over 60, it can occur at any age. It accounts for about 1% of all cancers and is the most common type of acute leukemia in adults. Advances in chemotherapy, targeted therapy, and stem cell transplantation have improved survival, but prognosis depends on age, genetic mutations, and response to treatment.
Commonly Associated with Acute Myeloid Leukaemia
AML is associated with several risk factors and conditions, including:
- Older age – most cases occur in people over 60.
- Previous chemotherapy or radiation therapy for another cancer.
- Genetic syndromes such as Down syndrome, Fanconi anemia, Bloom syndrome, and Li-Fraumeni syndrome.
- Blood disorders such as myelodysplastic syndromes (MDS) or myeloproliferative neoplasms (MPN).
- Exposure to chemicals like benzene or high-dose ionizing radiation.
- Family history of hematologic malignancies.
- Certain genetic mutations and chromosomal abnormalities, including FLT3, NPM1, CEBPA, and t(8;21).
Causes of Acute Myeloid Leukaemia
The exact cause of AML is not fully understood, but it arises when genetic mutations occur in the DNA of hematopoietic stem cells in the bone marrow. These mutations disrupt normal cell growth and differentiation, causing immature myeloid cells to multiply uncontrollably. Key contributing factors include:
- Acquired genetic mutations that activate oncogenes or disable tumor suppressor genes.
- Chromosomal translocations and deletions (e.g., inv[16], t[15;17]) that alter gene function.
- Inherited predispositions that impair DNA repair or regulation.
- Environmental exposures such as benzene or ionizing radiation.
- Therapy-related AML following chemotherapy or radiotherapy for prior cancers.
These abnormal myeloblasts crowd out healthy cells, leading to impaired blood cell production and rapid disease progression.
Symptoms of Acute Myeloid Leukaemia
Symptoms of AML typically develop over weeks and are due to bone marrow failure and infiltration of leukemic cells into various organs. Common signs and symptoms include:
- Anemia-related symptoms: Fatigue, weakness, pallor, and shortness of breath.
- Low white blood cell count: Frequent infections and fevers.
- Low platelet count: Easy bruising, petechiae, nosebleeds, and gum bleeding.
- Bone and joint pain: Due to expansion of the bone marrow.
- Swollen gums: Gingival hypertrophy, especially in monocytic subtypes.
- Swollen lymph nodes, liver, or spleen (less common than in ALL).
- Unexplained weight loss and night sweats.
- Leukostasis symptoms: Headache, confusion, or vision changes if white blood cell counts are extremely high.
Because AML progresses quickly, early recognition of these symptoms is critical.
Exams & Tests for Acute Myeloid Leukaemia
Diagnosis is based on clinical presentation, blood tests, and bone marrow examination:
- Complete blood count (CBC): Often shows anemia, thrombocytopenia, and abnormal white blood cell counts.
- Peripheral blood smear: Reveals circulating myeloblasts, often containing Auer rods (needle-like inclusions characteristic of AML).
- Bone marrow aspiration and biopsy: Confirms diagnosis with ≥20% blasts in the marrow.
- Immunophenotyping (flow cytometry): Identifies myeloid markers such as CD13, CD33, and MPO.
- Cytogenetic and molecular testing: Detects chromosomal abnormalities (e.g., t[15;17], inv[16]) and gene mutations (e.g., FLT3, NPM1) crucial for prognosis and treatment decisions.
- Lumbar puncture: Occasionally performed to check for central nervous system involvement in high-risk cases.
- Imaging: May be used to assess organ involvement if symptoms suggest infiltration.
Treatment of Acute Myeloid Leukaemia
Treatment for AML is urgent and typically involves two main phases: induction therapy to achieve remission and consolidation therapy to prevent relapse. The approach is tailored based on patient age, genetic risk, and disease subtype.
1. Induction Therapy
- Goal: Eliminate leukemic cells and achieve complete remission.
- Standard regimen: “7+3” chemotherapy – 7 days of cytarabine plus 3 days of an anthracycline (e.g., daunorubicin or idarubicin).
- In acute promyelocytic leukemia (APL), a distinct subtype, all-trans retinoic acid (ATRA) and arsenic trioxide are used instead of standard chemotherapy.
2. Consolidation Therapy
- Goal: Destroy residual leukemia cells and prevent relapse.
- Options: High-dose cytarabine, additional chemotherapy cycles, or allogeneic stem cell transplantation in high-risk patients.
3. Targeted Therapies
- FLT3 inhibitors (e.g., midostaurin)
- IDH1/IDH2 inhibitors (e.g., ivosidenib, enasidenib)
- BCL-2 inhibitor (venetoclax) for certain subtypes
4. Supportive Care
- Blood and platelet transfusions
- Antibiotics and antifungals to prevent infections
- Management of tumor lysis syndrome and leukostasis
5. Stem Cell Transplantation
- Considered for patients at high risk of relapse or with unfavorable genetic profiles.
Prognosis varies by age, genetic mutations, and response to therapy. Younger patients with favorable cytogenetics have 5-year survival rates of 50–70%, while rates are lower in older adults.
Source
- Döhner H, et al. “Diagnosis and management of AML in adults: 2017 ELN recommendations.” Blood 2017; 129(4):424–447.
- Ferrara F, Schiffer CA. “Acute myeloid leukaemia in adults.” Lancet 2013; 381(9865):484–495.
- National Cancer Institute. “Adult Acute Myeloid Leukemia Treatment (PDQ®) – Health Professional Version.” NCI, 2024.