Overview of Ankylosing Spondylitis
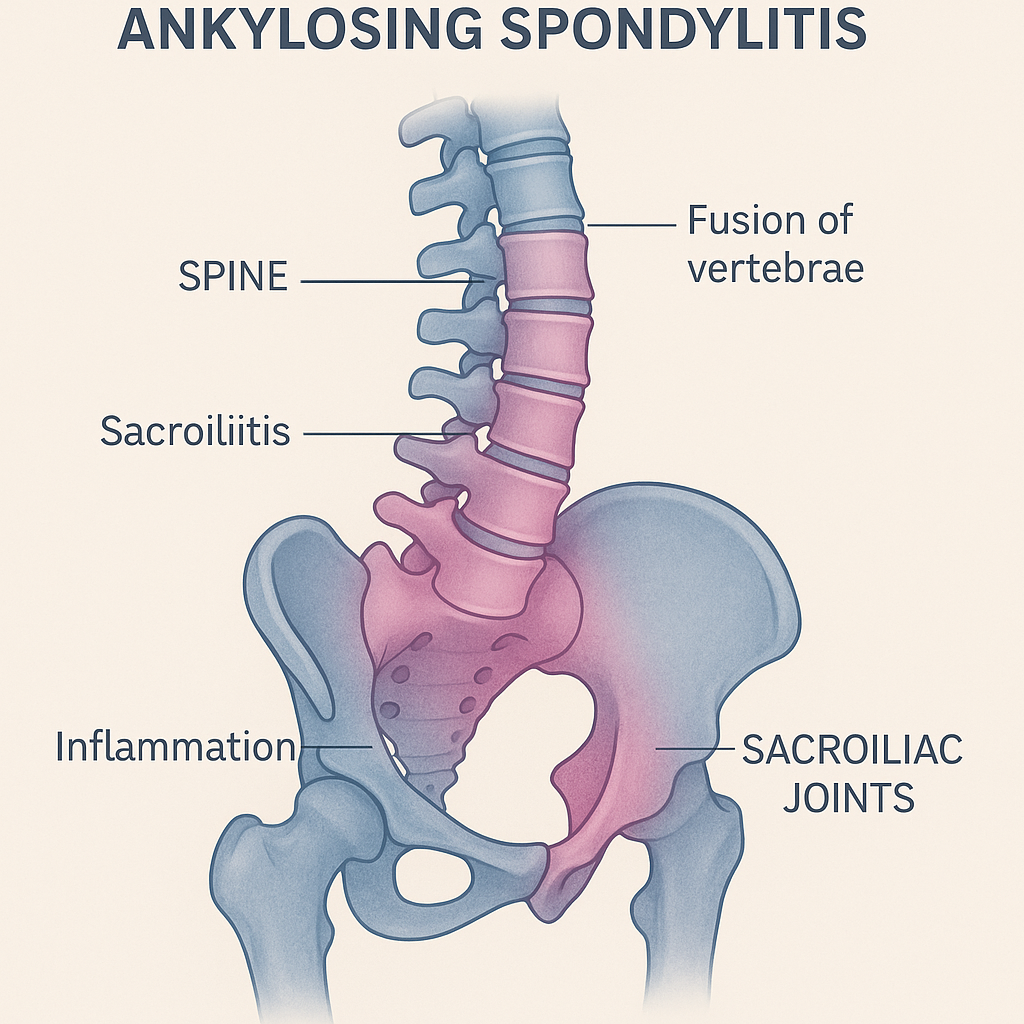
Ankylosing spondylitis (AS) is a chronic, progressive, inflammatory arthritis that primarily affects the axial skeleton, especially the spine and sacroiliac joints. Over time, inflammation leads to fusion of the vertebrae (ankylosis), resulting in stiffness, reduced mobility, and a characteristic forward-stooped posture. AS belongs to a group of conditions known as spondyloarthropathies and most commonly affects young men aged 20–40 years.
While the disease primarily targets the spine, it can also affect peripheral joints, eyes, skin, and cardiovascular system. Early diagnosis and intervention are crucial, as timely treatment can slow disease progression, reduce symptoms, and maintain quality of life.
Commonly Associated with Ankylosing Spondylitis
Several risk factors and conditions are strongly associated with ankylosing spondylitis:
- Genetic predisposition: Over 90% of patients carry the HLA-B27 gene.
- Age: Most cases develop in late adolescence to early adulthood.
- Sex: Men are affected more frequently and often more severely than women.
- Family history: First-degree relatives of affected individuals are at higher risk.
- Other spondyloarthropathies: Such as psoriatic arthritis, reactive arthritis, and inflammatory bowel disease–associated arthritis.
Causes of Ankylosing Spondylitis
The exact cause of AS is unknown, but it results from a combination of genetic, immune, and environmental factors:
- Genetic factors: The presence of the HLA-B27 gene significantly increases susceptibility, although not all carriers develop the disease.
- Immune dysregulation: Abnormal immune responses target ligaments and entheses (where ligaments and tendons attach to bone), causing chronic inflammation.
- Environmental triggers: Possible roles for gut microbiota, infections, or mechanical stress in triggering disease in genetically predisposed individuals.
The inflammatory process primarily affects the entheses, leading to bone erosion, followed by abnormal new bone formation and eventual spinal fusion.
Symptoms of Ankylosing Spondylitis
Symptoms typically develop gradually over several months or years and may initially be mistaken for mechanical back pain. Common signs and symptoms include:
- Chronic back pain and stiffness – especially in the lower back and buttocks, worse in the morning or after inactivity, improving with exercise.
- Reduced spinal flexibility – difficulty bending or twisting the back.
- Stooped posture – due to progressive spinal fusion.
- Pain and swelling in peripheral joints – hips, shoulders, knees.
- Enthesitis – inflammation where tendons and ligaments attach to bone (e.g., Achilles tendon).
- Chest pain or reduced chest expansion – due to involvement of costovertebral joints.
- Fatigue and weight loss.
Extra-articular manifestations:
- Uveitis (eye inflammation): Occurs in up to 40% of patients, causing eye pain, redness, and vision changes.
- Cardiovascular complications: Aortitis, aortic valve regurgitation.
- Pulmonary fibrosis: Rare but possible in advanced disease.
Exams & Tests for Ankylosing Spondylitis
Diagnosis is based on clinical features, imaging, and laboratory findings. Early detection is important to prevent irreversible damage.
- Medical history and physical examination: Focus on chronic back pain, stiffness, and reduced spinal mobility.
- Schober test: Measures lumbar spine flexibility.
- Chest expansion test: Assesses thoracic involvement.
Laboratory tests:
- HLA-B27 testing: Positive in most patients but not diagnostic on its own.
- Inflammatory markers: Elevated ESR and CRP levels may indicate active inflammation.
Imaging studies:
- X-rays: Reveal sacroiliitis (inflammation of the sacroiliac joints) and characteristic “bamboo spine” appearance in advanced stages.
- MRI: Detects early sacroiliac joint inflammation before changes appear on X-rays.
- CT scan: Occasionally used for detailed joint evaluation.
Treatment of Ankylosing Spondylitis
There is no cure for AS, but treatment aims to reduce inflammation, relieve pain, maintain spinal mobility, and prevent complications.
1. Medications:
- NSAIDs (e.g., naproxen, indomethacin): First-line therapy to relieve pain and inflammation.
- Biologic agents:
- TNF inhibitors (adalimumab, etanercept, infliximab) – highly effective for active disease.
- IL-17 inhibitors (secukinumab, ixekizumab) – alternatives for patients who do not respond to TNF blockers.
- Corticosteroid injections: For localized joint inflammation.
- DMARDs (e.g., sulfasalazine): Occasionally used for peripheral joint involvement.
2. Physical Therapy and Exercise:
- Daily stretching and posture exercises to maintain flexibility.
- Breathing exercises to preserve chest expansion.
- Hydrotherapy and low-impact activities (e.g., swimming) to strengthen muscles.
3. Lifestyle Modifications:
- Avoid smoking (linked to worse outcomes and lung complications).
- Maintain healthy weight and bone density.
- Ergonomic adjustments for posture and sleep.
4. Surgery:
- Joint replacement (e.g., hip arthroplasty): For severe joint damage.
- Corrective spinal surgery: Rare, for severe deformities.
Source
- Ward MM, et al. “2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Guidelines for the Treatment of Ankylosing Spondylitis.” Arthritis Rheumatol 2019; 71(10):1599–1613.
- Braun J, Sieper J. “Ankylosing spondylitis.” Lancet 2007; 369(9570):1379–1390.
- Poddubnyy D, et al. “Current diagnosis and treatment of ankylosing spondylitis.” Ther Adv Musculoskelet Dis 2021; 13:1759720X21995836.