Overview of Abdominal Aortic Aneurysm
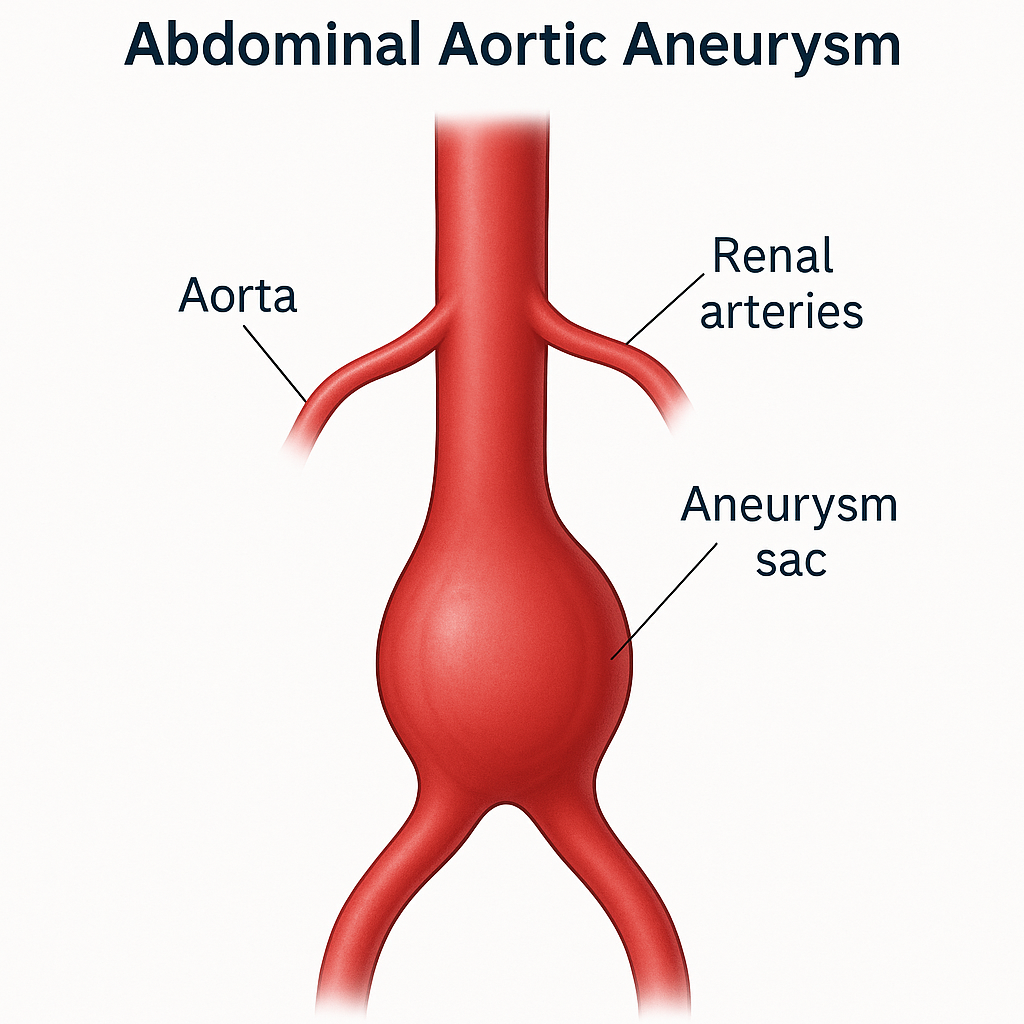
An abdominal aortic aneurysm (AAA) is an abnormal, localized enlargement of the abdominal aorta, the main blood vessel that supplies blood to the lower part of the body. This occurs when the wall of the aorta weakens and bulges outward, typically defined as an aortic diameter greater than 3 cm. Most AAAs develop slowly and without symptoms, often going undetected until they are discovered during imaging for unrelated reasons. However, if the aneurysm continues to expand, it can rupture, leading to catastrophic internal bleeding and a high risk of death. Early detection and careful monitoring are crucial, as ruptured AAAs carry a mortality rate exceeding 80%.
Conditions Commonly Associated with Abdominal Aortic Aneurysm
Several risk factors and conditions are strongly associated with the development of an abdominal aortic aneurysm:
- Atherosclerosis – buildup of fatty plaques that weaken arterial walls.
- Hypertension (high blood pressure) – places increased mechanical stress on the aorta.
- Smoking – a major modifiable risk factor that significantly raises AAA risk.
- Advanced age – most common in individuals over 65 years.
- Male sex – men are 4–5 times more likely to develop an AAA than women.
- Family history – first-degree relatives of patients with AAA have a higher risk.
- Connective tissue disorders – including Marfan and Ehlers-Danlos syndromes.
- Other vascular diseases – such as peripheral artery disease and coronary artery disease.
Causes of Abdominal Aortic Aneurysm
The exact cause of an abdominal aortic aneurysm is not always clear, but several underlying processes contribute to its formation:
- Degeneration of the aortic wall – age-related breakdown of elastin and collagen reduces vessel strength.
- Atherosclerosis – chronic plaque buildup and inflammation damage the arterial lining.
- Genetic predisposition – inherited connective tissue weaknesses make the aorta more vulnerable.
- Infections and inflammation – mycotic aneurysms or vasculitis can erode the vessel wall.
- Chronic high blood pressure – continuous mechanical stress accelerates dilation.
- Trauma or surgical injury – rarely, direct damage to the aorta can lead to aneurysm formation.
Symptoms of Abdominal Aortic Aneurysm
Most abdominal aortic aneurysms are asymptomatic and are discovered incidentally during imaging. When symptoms occur, they may include:
- A pulsating mass or sensation near the navel.
- Deep, constant abdominal or back pain that may radiate to the legs or buttocks.
- Abdominal tenderness or discomfort.
A ruptured AAA is a medical emergency. Symptoms may include:
- Sudden, severe abdominal or back pain.
- Low blood pressure, dizziness, or fainting.
- Loss of consciousness due to internal bleeding.
Immediate emergency treatment is crucial, as rupture is often fatal without rapid surgical intervention.
Exams & Tests for Abdominal Aortic Aneurysm
Since most AAAs develop without symptoms, screening and imaging are key to diagnosis. Common diagnostic tools include:
- Abdominal ultrasound – the first-line, non-invasive test for detecting and measuring aneurysms.
- CT scan (computed tomography) – offers detailed cross-sectional images and is essential for surgical planning.
- MRI (magnetic resonance imaging) – provides high-resolution anatomical detail in select cases.
- Physical examination – may detect a pulsatile abdominal mass, though sensitivity is low in obese patients.
Routine screening is recommended for men aged 65–75 who have ever smoked and for individuals with a family history of AAA.
Treatment of Abdominal Aortic Aneurysm
Management depends on the aneurysm’s size, growth rate, and symptoms:
- Observation and monitoring – Small aneurysms (<5.5 cm in men, <5.0 cm in women) are monitored regularly with imaging and managed through lifestyle modification and blood pressure control.
- Endovascular aneurysm repair (EVAR) – A minimally invasive procedure where a stent-graft is inserted through the femoral artery and placed inside the aneurysm to reinforce the vessel wall.
- Open surgical repair – Involves removing the aneurysmal section and replacing it with a synthetic graft, typically recommended for large or symptomatic aneurysms or in emergencies.
Emergency surgery for a ruptured abdominal aortic aneurysm is lifesaving but carries a significant risk, even with rapid intervention.
Sources