Overview of Addison’s Disease
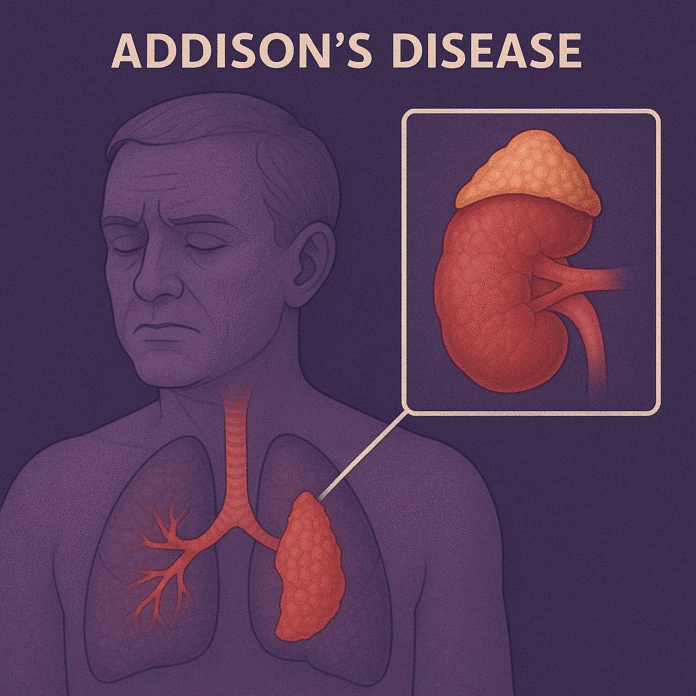
Addison’s disease, also known as primary adrenal insufficiency, is a rare endocrine disorder that occurs when the adrenal glands — located atop the kidneys — fail to produce sufficient amounts of the hormones cortisol and aldosterone. These hormones are essential for regulating metabolism, immune function, blood pressure, and the body’s response to stress.
The condition develops gradually but can become life-threatening if not treated, particularly during times of stress or illness. It affects people of all ages and sexes, though it is most commonly diagnosed in adults aged 30–50 years. Early diagnosis and proper hormone replacement therapy allow most people with Addison’s disease to lead normal, healthy lives.
Commonly Associated With Addison’s Disease
Addison’s disease is often linked to the following risk factors and conditions:
- Autoimmune diseases – the most common cause, often occurring alongside autoimmune thyroid disease or type 1 diabetes (autoimmune polyglandular syndrome).
- Chronic infections – such as tuberculosis, HIV/AIDS, or fungal infections that damage the adrenal glands.
- Adrenal hemorrhage or infarction – often associated with severe sepsis or anticoagulant use.
- Metastatic cancer – spread of cancer from other organs to the adrenal glands.
- Genetic conditions – such as adrenoleukodystrophy.
- Prolonged use of corticosteroids – abrupt withdrawal can trigger secondary adrenal insufficiency.
Causes of Addison’s Disease
Addison’s disease occurs when 90% or more of the adrenal cortex is destroyed, impairing its ability to produce cortisol and aldosterone. The causes are categorized as primary (damage to the adrenal glands) or, less commonly, secondary (pituitary or hypothalamic dysfunction).
Primary causes (most common):
- Autoimmune adrenalitis – the immune system attacks the adrenal cortex, accounting for ~70–80% of cases.
- Infections – particularly tuberculosis, which remains a major cause in developing countries.
- Metastatic cancer – such as lung, breast, or melanoma invading adrenal tissue.
- Adrenal hemorrhage or infarction – due to severe infections (e.g., meningococcemia) or clotting disorders.
Secondary adrenal insufficiency (not classic Addison’s):
- Pituitary or hypothalamic disorders leading to low ACTH production.
- Sudden withdrawal of long-term corticosteroid therapy.
Symptoms of Addison’s Disease
Symptoms of Addison’s disease typically develop gradually and may go unnoticed until they become severe. Common signs and symptoms include:
- Chronic fatigue and muscle weakness
- Unexplained weight loss and loss of appetite
- Low blood pressure, sometimes causing dizziness or fainting
- Hyperpigmentation – darkening of skin, particularly in skin creases, scars, and mucous membranes (due to elevated ACTH)
- Salt cravings – from low aldosterone leading to sodium loss
- Nausea, vomiting, diarrhea, or abdominal pain
- Irritability, depression, or mood changes
- Low blood sugar (hypoglycemia) – especially in children
- Dehydration and electrolyte imbalance – low sodium and high potassium levels
A sudden worsening known as an Addisonian crisis can occur during severe stress or illness, leading to shock, severe hypotension, confusion, and possible death without immediate treatment.
Exams & Tests for Addison’s Disease
Diagnosis involves blood tests, hormone stimulation tests, and imaging to assess adrenal function and structure.
- Blood tests:
- Low cortisol and aldosterone levels.
- High adrenocorticotropic hormone (ACTH) levels (in primary adrenal insufficiency).
- Low sodium and high potassium levels.
- ACTH stimulation test (cosyntropin test):
- Measures cortisol response after synthetic ACTH injection. Little or no increase confirms adrenal insufficiency.
- Plasma renin activity and aldosterone:
- Help assess mineralocorticoid deficiency.
- Antibody tests:
- Detect autoimmune adrenalitis.
- Imaging:
- CT scan of adrenal glands to look for calcifications (tuberculosis), hemorrhage, or tumors.
- MRI of the pituitary if secondary adrenal insufficiency is suspected.
Treatment of Addison’s Disease
Treatment focuses on replacing the deficient hormones and managing symptoms. With proper therapy, most patients can live normal, active lives.
1. Hormone Replacement Therapy:
- Glucocorticoids – Hydrocortisone, prednisone, or dexamethasone to replace cortisol.
- Mineralocorticoids – Fludrocortisone to replace aldosterone and help regulate blood pressure and electrolytes.
2. Stress-Dose Adjustments:
- Increased glucocorticoid doses during illness, surgery, or stress to prevent adrenal crisis.
3. Addisonian Crisis Management:
- Emergency IV hydrocortisone, saline, and dextrose to restore blood pressure and electrolyte balance.
4. Lifestyle and Monitoring:
- Regular follow-up and blood tests to monitor hormone levels.
- Wearing a medical alert bracelet.
- Carrying an emergency injectable hydrocortisone kit.
Source
- Bornstein SR, et al. “Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline.” J Clin Endocrinol Metab 2016; 101(2):364–389.
- Husebye ES, et al. “Adrenal insufficiency.” Lancet 2021; 397(10274):613–629.
- National Institute for Health and Care Excellence (NICE). “Adrenal insufficiency: diagnosis and management.” NICE Guideline NG321, 2023.