Overview
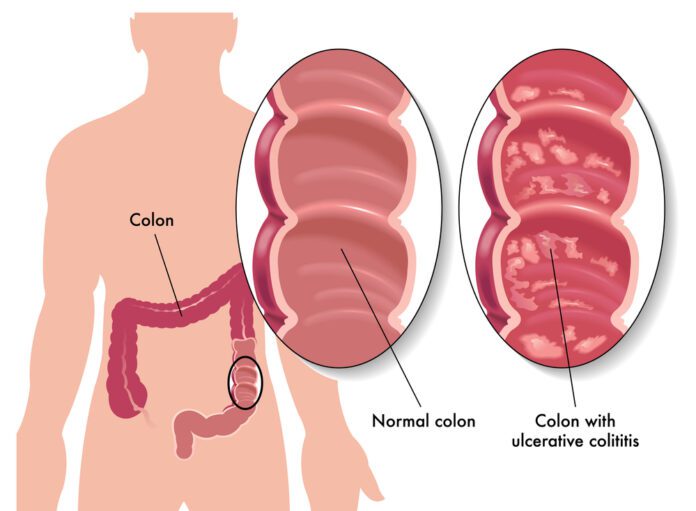
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes the lining of the colon and rectum to become inflamed.
The disease begins in the rectal area and can spread to higher areas of the colon. Crohn’s disease is a condition related to Ulcerative colitis.
Cause
The cause of ulcerative colitis remains unknown.
People with this disease develop problems with their immune systems, though it is unclear if immune problems cause this illness.
Though symptoms of ulcerative colitis can be triggered by stress and certain foods, they do not cause the illness.
Ulcerative colitis can affect any age group however, ages 15 to 30 and 50 to 70 are most at risk.
A family history of ulcerative colitis, other autoimmune diseases, or Jewish ancestry are among the risk factors for this disease.
Symptoms
Ulcerative colitis symptoms vary in intensity.
Half of the people with this disease only have mild symptoms whilst others face more severe symptoms that flare up more often.
Symptoms may include:
- Abdominal pain and cramping.
- A splashing sound heard around the intestine.
- Blood and pus in stools.
- Diarrhea.
- Fever.
- Tenesmus.
- Weight loss.
- Stunted growth in children.
- Swollen joints.
- Mouth sores (ulcers).
- Nausea and vomiting.
- Skin lumps or ulcers.
Exams and Tests
A colonoscopy with a biopsy is often used to diagnose the disease. It is also used to screen people with ulcerative colitis for colon cancer.
A CT scan, MRI, upper endoscopy or MR enterography is sometimes need to differentiate between ulcerative colitis and Crohn disease.
Other tests to help diagnose this condition include:
- Barium enema.
- Stool calprotectin or lactoferrin.
- Erythrocyte sedimentation rate (ESR).
- Complete blood count (CBC).
- Antibody tests by blood.
Sometimes, tests are needed to differentiate between ulcerative colitis and Crohn disease, including:
- A CT scan.
- An MRI.
- An upper endoscopy or capsule study.
- An MR enterography.
Treatment
The goal of treatment is to:
- Help the colon heal.
- Control acute attacks.
- Prevent repeated attacks.
During a severe attack, you may need treatment at a hospital.
Your doctor may prescribe corticosteroids as well as administer nutrients through via an IV line.
Diet and Nutrition
Certain foods may worsen diarrhea and gas symptoms. This problem may be more severe when the disease is active.
Suggested for your diet include:
- Small food portions.
- Avoid food with high-fiber (bran, beans, nuts, seeds, and popcorn).
- Drink plenty of water.
- Avoid greasy or fried foods and sauces (butter, margarine, and heavy cream).
- Reduce milk products (if you are lactose intolerant persons).
STRESS
Stressful events in your life such losing a job or a loved one can also worsen digestive problems.
Seek tips from your health care provider on how to manage your stress.
MEDICINES
Medicines that may be used to decrease ulcerative colitis attacks include:
- 5-aminosalicylates such as mesalamine or sulfasalazine to help control moderate symptoms.
- Medicines to calm the immune system.
- Corticosteroids such as prednisone.
- Immunomodulators such as azathioprine and 6-MP.
- Biologic therapy, if other drugs do not work.
- Acetaminophen (Tylenol) to help relieve mild pain.
Avoid drugs that worsen symptoms such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn).
SURGERY
Surgery to remove the colon will cure ulcerative colitis and also remove the threat of colon cancer.
You may need surgery if:
- Medical therapy is innefective against the Colitis.
- There are changes in the lining of the colon, which suggest an increased risk of cancer
- There are severe problems, such as toxic megacolon, a rupture of the colon, or severe bleeding.
Most of the time, the entire colon, including the rectum, is removed during the surgery.
After surgery, you may have an opening in your belly called the stoma (ileostomy) which your stool will drain out of.
You will also have a procedure that connects the small intestine to the anus to gain more normal bowel function.
Exams and Tests
Your healthcare provider will perform a physical exam on you as well as ask questions about your symptoms such as:
- How long have you had the symptoms?
- Whether you have been travelling?
- If you have recently taken antibiotics?
- How often you have pain?
- What the severity of the pain is?
- How often you have diarrhea?
Your healthcare provider may recommend a colonoscopy or a flexible sigmoidoscopy. A flexible tube is inserted through the rectum to examine the colon during this test.
You may have biopsies taken during this exam which may show changes related to inflammation.
A CT scan of the abdomen, a barium enema, an MRI of the abdomen, stool culture and stool examination for ova and parasites can also identify colitis.