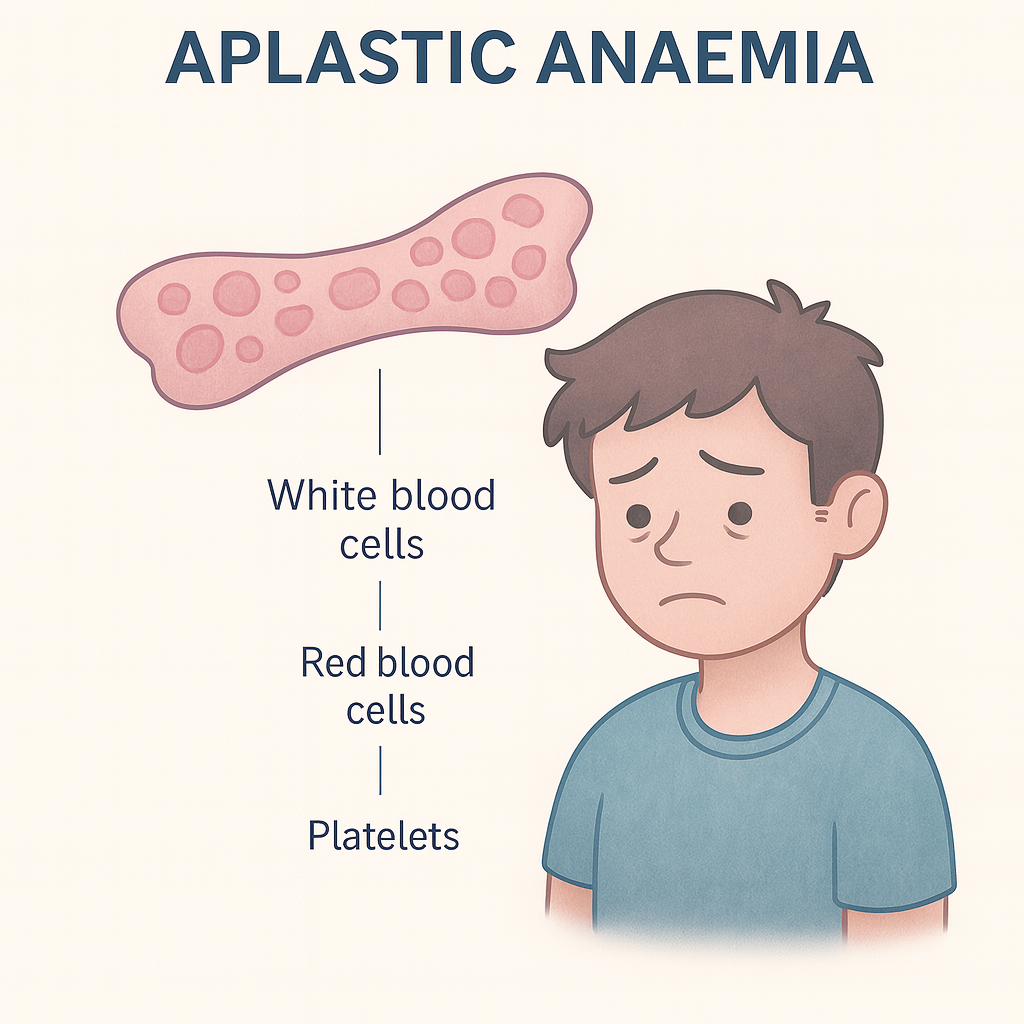
Overview of Aplastic Anaemia
Aplastic anaemia is a rare but serious blood disorder in which the bone marrow fails to produce enough blood cells — including red blood cells, white blood cells, and platelets. This leads to pancytopenia (a deficiency of all three types of blood cells), causing fatigue, increased risk of infections, and bleeding tendencies.
The condition can occur at any age but is most common in adolescents, young adults, and older adults over 60. Aplastic anaemia may develop suddenly (acute) or gradually (chronic). Without prompt diagnosis and treatment, severe cases can be life-threatening, but many patients respond well to therapies such as immunosuppressive treatment or stem cell transplantation.
Commonly Associated with Aplastic Anaemia
Several factors and conditions are commonly linked with aplastic anaemia:
- Autoimmune diseases – the most frequent cause in developed countries.
- Exposure to toxic chemicals – such as benzene, pesticides, or solvents.
- Certain medications – including chemotherapy drugs, chloramphenicol, and some antiepileptics.
- Radiation exposure – accidental or therapeutic.
- Viral infections – particularly hepatitis viruses, Epstein-Barr virus (EBV), cytomegalovirus (CMV), and HIV.
- Inherited bone marrow failure syndromes – e.g., Fanconi anaemia, Shwachman-Diamond syndrome.
- Pregnancy – rarely, immune changes during pregnancy can trigger aplastic anaemia.
In many cases, the cause is idiopathic (unknown).
Causes of Aplastic Anaemia
The main cause is damage to the hematopoietic stem cells in the bone marrow, which impairs their ability to produce blood cells. This damage can result from:
- Autoimmune attack: The body’s immune system mistakenly targets bone marrow stem cells, destroying them.
- Toxins and chemicals: Long-term exposure to benzene, pesticides, or heavy metals can suppress bone marrow function.
- Medications: Certain drugs can trigger bone marrow suppression as an adverse effect.
- Radiation or chemotherapy: These treatments damage rapidly dividing cells, including those in the bone marrow.
- Infections: Viral infections (especially hepatitis) can directly damage stem cells or trigger immune-mediated destruction.
- Inherited conditions: Genetic disorders such as Fanconi anaemia cause defective DNA repair, leading to marrow failure.
Symptoms of Aplastic Anaemia
Symptoms arise due to deficiencies of red blood cells, white blood cells, and platelets. They may develop gradually or appear suddenly in severe cases.
Low red blood cells (anaemia):
- Fatigue and weakness
- Shortness of breath
- Pale skin (pallor)
- Dizziness or fainting
- Rapid or irregular heartbeat
Low white blood cells (leukopenia):
- Frequent or severe infections
- Fever and sore throat
Low platelets (thrombocytopenia):
- Easy bruising
- Prolonged bleeding from cuts
- Nosebleeds or bleeding gums
- Petechiae (small red spots on the skin)
Severe aplastic anaemia can lead to life-threatening infections or uncontrolled bleeding if not treated promptly.
Exams & Tests for Aplastic Anaemia
Diagnosis requires a combination of blood tests and bone marrow analysis:
- Complete blood count (CBC):
- Low red blood cells, white blood cells, and platelets (pancytopenia).
- Normal cell morphology (cells appear normal but are reduced in number).
- Reticulocyte count:
- Low reticulocyte count, indicating reduced new red blood cell production.
- Bone marrow biopsy:
- Hypocellular marrow with reduced or absent hematopoietic cells and increased fat spaces — the hallmark of aplastic anaemia.
- Additional tests:
- Liver function tests – to check for viral hepatitis.
- Viral serologies – to detect EBV, CMV, HIV, or hepatitis viruses.
- Chromosomal analysis – to rule out inherited bone marrow failure syndromes.
- Flow cytometry (PNH screen): To detect paroxysmal nocturnal hemoglobinuria, which can coexist with aplastic anaemia.
Treatment of Aplastic Anaemia
Treatment depends on the severity of the condition, the patient’s age, and the underlying cause. The main goals are to restore normal blood cell production, manage complications, and prevent infections.
1. Supportive Care:
- Blood transfusions: Red cells and platelets to treat anaemia and bleeding.
- Antibiotics and antivirals: To prevent or treat infections.
- Growth factors (e.g., G-CSF): Stimulate white blood cell production in some cases.
2. Immunosuppressive Therapy:
- Standard for patients who are not transplant candidates.
- Antithymocyte globulin (ATG) and cyclosporine suppress immune-mediated destruction of stem cells.
- Eltrombopag: A thrombopoietin receptor agonist that stimulates blood cell production.
3. Hematopoietic Stem Cell Transplantation (HSCT):
- Curative treatment for severe aplastic anaemia, especially in patients under 40 with a matched sibling donor.
- Replaces damaged bone marrow with healthy stem cells to restore blood cell production.
4. Treating Underlying Causes:
- Discontinuing causative medications.
- Treating infections or removing exposure to toxic chemicals.
Prognosis:
With modern treatments, 5-year survival exceeds 80% in younger patients receiving stem cell transplants. Older patients or those without a donor also achieve high survival rates with immunosuppressive therapy.
Source
- Killick SB, et al. “Guidelines for the diagnosis and management of adult aplastic anaemia.” Br J Haematol 2022; 196(6):1389–1407.
- Townsley DM, et al. “Aplastic anemia: pathophysiology and treatment.” Hematology Am Soc Hematol Educ Program 2020; 2020(1):52–60.
- Young NS. “Aplastic anemia.” N Engl J Med 2018; 379(17):1643–1656.