Overview
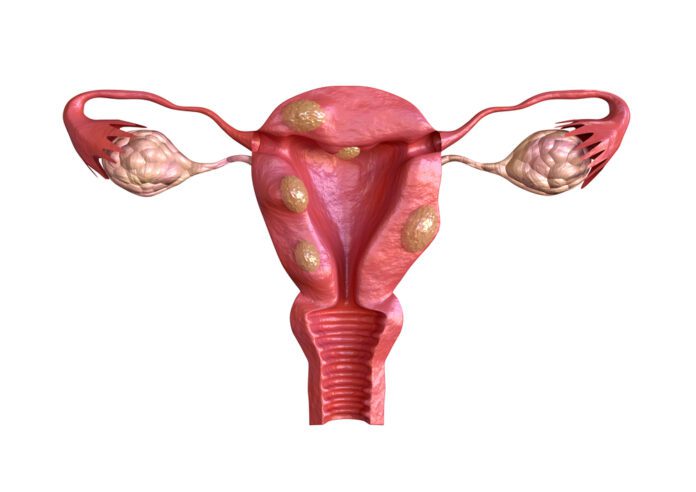
Uterine fibroids are growths made of smooth muscle cells, fibroblasts, and other materials that grow in or on the wall of the uterus.
Fibroids may grow as a single tumor or in clusters. In many cases, a single uterus contains many fibroids.
Fibroids can be of different sizes or shapes. Bunches or clusters of fibroids are often of different sizes. Fibroids can grow, shrink, or remain a constant size over time.
Health care providers categorize fibroids based on where they grow:
● Submucosal fibroids grow just underneath the uterine lining and into the endometrial cavity.
● Intramural fibroids grow in between the muscles of the uterus.
● Subserosal fibroids grow on the outside of the uterus.
Some fibroids grow on stalks that grow out from the surface of the uterus or into the uterine cavity. These are called pedunculated fibroids.
Commonly Associated With
Leiomyoma; Fibromyoma; Myoma; Fibroids; Uterine bleeding – fibroids; Vaginal bleeding – fibroids
Cause
Uterine fibroids are common. As many as one in five women may have fibroids during their childbearing years. Half of all women have fibroids by age 50.
Fibroids are rare in women under age 20. They are more common in African Americans than White, Hispanic, or Asian women.
No one knows exactly what causes fibroids. They are thought to be caused by:
• Hormones in the body
• Genes (may run in families)
Fibroids can be so tiny that you need a microscope to see them. They can also grow very large. They may fill the entire uterus and may weigh several pounds or kilograms. Although it is possible for just one fibroid to develop, most often there is more than one.
Fibroids can grow:
• In the muscle wall of the uterus (myometrial)
• Just under the surface of the uterine lining (submucosal)
• Just under the outside lining of the uterus (subserosal)
• On a long stalk on the outside the uterus or inside the uterus (pedunculated)
Symptoms
Many women have no symptoms of fibroids. However, uterine fibroids can cause uncomfortable or sometimes painful symptoms, such as:
● Heavy bleeding or painful periods
● Anemia (when you don’t have enough red blood cells)
● Bleeding between periods
● Feeling “full” in the lower abdomen (belly)—this is sometimes called pelvic pressure
● Frequent urination (caused by a fibroid pressing on the bladder)
● Pain during sex
● Lower back pain
● Reproductive problems, such as infertility, multiple miscarriages, and early onset of labor during pregnancy
● Obstetrical problems, such as the increased likelihood of cesarean section
Treatment
Treatments for fibroids include the following:
● Medication-related treatments
● Other treatments
This page also includes information about emotional support for living with fibroids.
Your health care provider will consider several factors before recommending treatment for your fibroids, including:
● Your age
● Your general health
● How severe your symptoms are
● Where your fibroids are located
● The type and size of the fibroids
● Whether you are pregnant now or want to get pregnant in the future
If you have uterine fibroids but have no symptoms or problems, you may not need treatment. You can ask your health care provider to continue to check the fibroids at your routine gynecological exams to see whether they have grown. If you are close to menopause, your health care provider may find that your fibroids are shrinking, which is common during and after menopause.
Medication-Related Treatments for Fibroids
Depending on your symptoms, your health care provider may suggest medical treatments that can reduce the symptoms of fibroids or stop their growth. Certain medical treatments to reduce fibroid size and blood loss may be used in combination with other treatments.
Common medical treatments for fibroids include:
● Pain medicine. Over-the-counter or prescription medicine is often used for mild or occasional pain from fibroids.
● Birth control pills or other types of hormonal birth control. These medicines help control heavy bleeding and painful periods. However, this therapy can sometimes cause fibroids to grow larger.
● Progestin-releasing intrauterine device (IUD). The hormonal IUD, also called intrauterine contraception (IUC), reduces heavy and painful bleeding but does not treat the fibroids themselves. It is not recommended for women who have very large fibroids, which can block the uterine cavity.
● Gonadotropin-releasing hormone agonists (GnRHa). These medicines block the body from making the hormones that cause women to ovulate and have their periods. The medicines also reduce the size of fibroids. Because this treatment can cause side effects that mimic the symptoms of menopause (such as hot flashes, night sweats, and vaginal dryness) and bone loss (which weakens the bones), it is not meant for long-term use. Most of the time, these medicines are used for a short time to reduce the size of fibroids before surgery or to treat anemia. If you need to take this treatment for a long time, the doctor may prescribe different medicine to put back the hormones that were blocked.
● Antihormonal agents or hormone modulators (such as selective progesterone receptor modulators). These drugs, which include ulipristal acetate, mifepristone, and letrozole, can slow or stop the growth of fibroids, reduce bleeding, and improve symptoms.
Medical treatments may give only temporary relief from the symptoms of fibroids. Once you stop the treatment, fibroids can grow back and symptoms can return.
Medicines are generally safe, but they can have side effects, some of which may be serious. Be sure to talk to your health care provider about the possible side effects of any medical treatment you consider.
Hysterectomy
Hysterectomy is the only sure way to cure uterine fibroids completely. Health care providers may recommend this option if you are near or past menopause and you have large fibroids or very heavy bleeding.
During a hysterectomy, the whole uterus or just part of it is removed.
There are several ways to perform a hysterectomy:
● Abdominal hysterectomy. The surgeon removes the uterus through a cut in the abdomen. This incision may be similar to what is done during a cesarean section. This type of hysterectomy requires a longer hospital stay and longer recovery time than others.1 Removal of the ovaries is not required for the treatment of fibroid symptoms. Similarly, some women may desire to preserve the cervix if there is no history of abnormal Pap smears.
● Vaginal hysterectomy. Instead of making a cut into the abdomen, the surgeon removes the uterus through the vagina. This method is less invasive than an abdominal hysterectomy, so recovery time is usually shorter (3 to 4 weeks). Vaginal hysterectomy may not be an option if your fibroids are very large.
● Laparoscopic hysterectomy. Minimally invasive approaches include laparoscopic hysterectomy, laparoscopy-assisted vaginal hysterectomy, and robotic-assisted laparoscopic hysterectomy. Not all cases of uterine fibroids can be treated with such approaches, but these methods may result in reduced postoperative recovery time.
● Robotic hysterectomy. Robotic hysterectomy is becoming more common. The surgeon sits at a console near the patient and guides a robotic arm to perform laparoscopic surgery. Like laparoscopic myomectomies, this technique requires only small incisions in the uterus and abdomen. As a result, recovery can be shorter (3 to 4 weeks) than with more invasive procedures. More research is needed to understand how (and how well) these procedures work and to compare the outcomes with those of other established surgical treatments.
If you have not gone through menopause and are considering a hysterectomy for your fibroids, talk to your health care provider about keeping your ovaries. The ovaries make hormones that help maintain bone density and sexual health even if the uterus is removed. If your body can continue to make these hormones on its own, you might not need hormone replacement after the hysterectomy.
Having a hysterectomy means that you will no longer be able to get pregnant.3 This process cannot be reversed, so be certain about your choice before having the surgery
Other Treatments for Fibroids
Uterine fibroids can be treated with radiological and other methods. These can include endometrial ablation, uterine artery embolization, magnetic resonance imaging-guided focused ultrasound, and myomectomy.
These treatments are minimally invasive and typically involve a short hospital stay or can be done as an outpatient procedure. Before undergoing any treatment for uterine fibroids, you should discuss your options with your health care provider.
Exams and Tests
Your provider will perform a pelvic exam. This may show that you have a change in the shape of your womb.
Fibroids are not always easy to diagnose. Being obese may make fibroids harder to detect. You may need these tests to look for fibroids:
• Ultrasound uses sound waves to create a picture of the uterus.
• MRI uses powerful magnets and radio waves to create a picture.
• Saline infusion sonogram (hysterosonography) — Saline is injected into the uterus to make it easier to see the uterus using ultrasound.
• Hysteroscopy uses a long, thin tube inserted through the vagina and into the uterus to examine the inside of the uterus.
• Endometrial biopsy removes a small piece of the lining of the uterus to check for cancer if you have unusual bleeding.
Source
https://www.nichd.nih.gov/health/topics/uterine/conditioninfo
https://www.nichd.nih.gov/health/topics/uterine/conditioninfo/treatments