Overview
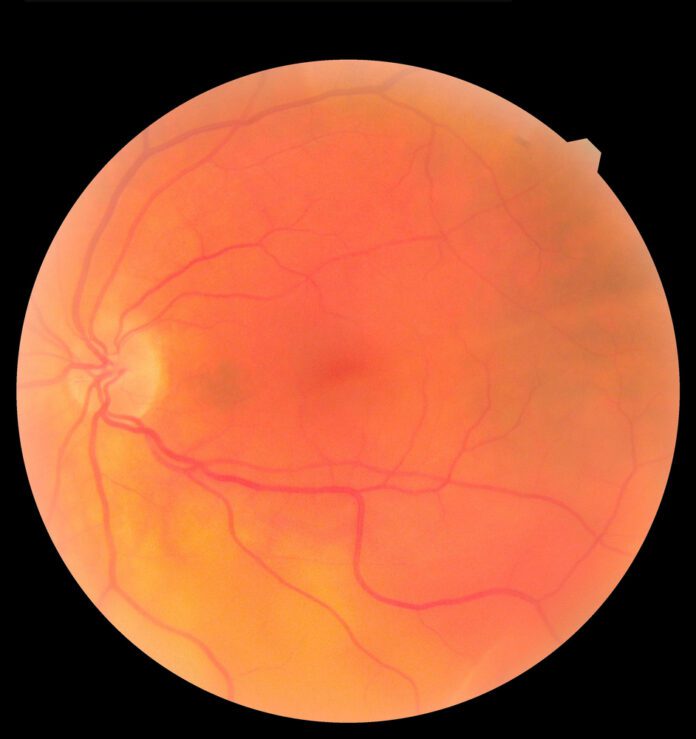
Macular edema is the build-up of fluid in the macula, an area in the center of the retina. The retina is the light-sensitive tissue at the back of the eye and the macula is the part of the retina responsible for sharp, straight-ahead vision. Fluid buildup causes the macula to swell and thicken, which distorts vision.
Cause
Macular edema occurs when there is abnormal leakage and accumulation of fluid in the macula from damaged blood vessels in the nearby retina. A common cause of macular edema is diabetic retinopathy, a disease that can happen to people with diabetes. Macular edema can also occur after eye surgery, in association with age-related macular degeneration, or as a consequence of inflammatory diseases that affect the eye. Any disease that damages blood vessels in the retina can cause macular edema.
Symptoms
The primary symptom of macular edema is blurry or wavy vision near or in the center of your field of vision. Colors might also appear washed out or faded. Most people with macular edema will have symptoms that range from slightly blurry vision to noticeable vision loss. If only one eye is affected, you may not notice your vision is blurry until the condition is well-advanced.
Treatment
How will my eye doctor check for macular edema?
To diagnose macular edema, your eye care professional will conduct a thorough eye exam and look for abnormalities in the retina. The following tests may be done to determine the location and extent of the disease:
Visual acuity test. A visual acuity test is a common way to identify vision loss and can help to diagnose vision loss as a result of macular edema. This test uses a standardized chart or card with rows of letters that decrease in size from top to bottom. Covering one eye, you will be asked to read out loud the smallest line of letters that you can see. When done, you will test the other eye.
Dilated eye exam. A dilated eye exam is used to more thoroughly examine the retina. It gives additional information about the condition of the macula and helps detect the presence of blood vessel leakage or cysts. Drops are placed in your eyes to widen, or dilate, your pupils. Your eye care professional then examines your retina for signs of damage or disease.
Fluorescein angiogram. If earlier tests indicate you could have macular edema, your eye care professional may perform a fluorescein angiogram. In this test, a special dye is injected into your arm and a camera takes photos of the retina as the dye travels through the blood vessels. This test helps your ophthalmologist identify the amount of damage to the macula.
Optical coherence tomography. This is a test that uses a special light and a camera for detailed views of the cell layers inside the retina. It detects the thickness of the retina and so it’s useful in determining the amount of swelling in the macula. Your eye care professional may also use optical coherence tomography after your treatment to track how well you are healing.
The Amsler Grid. The Amsler Grid provides an easy way to test whether or not your central vision has changed. It can recognize even small changes in your vision.
Other
Diabetic macular edema (DME)
Diabetic macular edema (DME) is caused by a complication of diabetes called diabetic retinopathy. Diabetic retinopathy is the most common diabetic eye disease and the leading cause of irreversible blindness in working-age Americans. Diabetic retinopathy usually affects both eyes.
Diabetic retinopathy is caused by ongoing damage to the small blood vessels of the retina. The leakage of fluid into the retina may lead to swelling of the surrounding tissue, including the macula.
DME is the most common cause of vision loss in people with diabetic retinopathy. Poor blood sugar control and additional medical conditions, such as high blood pressure, increase the risk of blindness for people with DME. DME can occur at any stage of diabetic retinopathy, although it is more likely to occur later as the disease goes on.
Experts estimate that approximately 7.7 million Americans have diabetic retinopathy and of those, about 750,000 also have DME. A recent study suggests that non-Hispanic African Americans are three times more likely to develop DME than non-Hispanic whites, most likely due to the higher incidence of diabetes in the African American population.
Eye surgery
Macular edema may develop after any type of surgery that is performed inside the eye, including surgery for cataract, glaucoma, or retinal disease. A small number of people who have cataract surgery (experts estimate only 1-3 percent) may develop macular edema within a few weeks after surgery. If one eye is affected, there is a 50 percent chance that the other eye will also be affected. Macular edema after eye surgery is usually mild, short-lasting, and responds well to eye drops that treat inflammation.
Age-related macular degeneration
Age-related macular degeneration (AMD) is a disease characterized by deterioration or breakdown of the macula, which is responsible for sharp, central vision. In neovascular AMD, also called “wet” AMD, blood vessels begin to grow up from the choroid (the bed of blood vessels below the retina) and into the retina. These new and abnormal blood vessels leak fluid into the macula and cause macular edema.
Blockage of retinal blood vessels
When retinal veins are blocked (retinal vein occlusion), blood does not drain properly and it leaks into the retina. If it leaks into the macula, this produces macular edema. Leakage is worsened by the severity of the blockage, how many veins are involved, and the pressure inside them. Retinal vein occlusion is most often associated with age-related atherosclerosis, diabetes, high blood pressure, and eye conditions such as glaucoma or inflammation.
Inflammatory diseases that affect the retina
Uveitis describes a group of inflammatory diseases that cause swelling in the eye and destroy eye tissues. The term “uveitis” is used because the diseases most often affect a part of the eye called the uvea. However, uveitis is not limited to the uvea. Uveitis can affect the cornea, iris, lens, vitreous, retina, optic nerve, and the white of the eye (sclera).
Inflammatory diseases and disorders of the immune system may also affect the eye and cause swelling and breakdown of tissue in the macula. These disorders include cytomegalovirus infection, retinal necrosis, sarcoidosis, Behçet’s syndrome, toxoplasmosis, Eales’ disease, and Vogt-Koyanagi-Harada syndrome
Source
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/macular-edema