Uses
Tacrolimus (Astagraf XL, Envarsus XR, Prograf) is used along with other medications to prevent rejection (attack of a transplanted organ by the immune system of a person receiving the organ) in people who have received a kidney transplant. Tacrolimus (Prograf) is also used along with other medications to prevent rejection in people who have received a liver or heart transplant. Tacrolimus is in a class of medications called immunosuppressants. It works by decreasing the activity of the immune system to prevent it from attacking the transplanted organ.
Side Effects Of Tacrolimus
Tacrolimus may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- headache
- diarrhea
- constipation
- nausea
- vomiting
- heartburn
- stomach pain
- loss of appetite
- difficulty falling asleep or staying asleep
- dizziness
- weakness
- back or joint pain
- burning, numbness, pain, or tingling in the hands or feet
Some side effects can be serious. If you experience any of the following symptoms or those mentioned in the IMPORTANT WARNING section, call your doctor immediately:
- decreased urination
- pain or burning on urination
- shortness of breath, hives, rash, or itching
- pale skin, shortness of breath, or fast heartbeat
- tiredness; weight gain; swelling of the arms, hands, feet, ankles, or lower legs; or shortness of breath
- unusual bleeding or bruising
- seizures, vision changes, headache, confusion, or uncontrollable shaking of a part of the body
- coma (loss of consciousness for a period of time)
Tacrolimus may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
Warnings & Precautions
Before taking tacrolimus:
- tell your doctor and pharmacist if you are allergic to tacrolimus, any other medications, or any of the other ingredients in tacrolimus products. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take with tacrolimus. Be sure to mention any of the following: amiodarone (Nexterone, Pacerone); amphotericin B (Abelcet, Ambisome); angiotensin-converting enzyme (ACE) inhibitors such as benazepril (Lotensin, in Lotrel), captopril, enalapril (Vasotec, in Vaseretic), fosinopril, lisinopril (in Prinzide, in Zestoretic), moexipril (Univasc, in Uniretic), perindopril (Aceon, in Prestalia), quinapril (Accupril, in Quinaretic), ramipril (Altace), or trandolapril (in Tarka); antacids containing magnesium and aluminum hydroxide (Maalox); certain antibiotics including aminoglycosides such as amikacin, gentamicin, neomycin (Neo-Fradin), streptomycin, and tobramycin (Tobi), and macrolides such as clarithromycin (Biaxin), erythromycin (EES, E-Mycin, Erythrocin), and troleandomycin (TAO; not available in the US); antifungal medications such as clotrimazole (Lotrimin, Mycelex), fluconazole (Diflucan), itraconazole (Onmel, Sporanox), ketoconazole, posaconazole (Noxafil), and voriconazole (Vfend); angiotensin receptor blockers (ARBs) such as azilsartan (Edarbi, in Edarbyclor), candesartan (Atacand, in Atacand HCT), eprosartan (Teveten), irbesartan (Avapro, in Avalide), losartan (Cozaar, in Hyzaar), olmesartan (Benicar, in Azor, in Benicar HCT, in Tribenzor), telmisartan (Micardis, in Micardis HCT, in Twynsta); boceprevir (Victrelis; no longer available in U.S.); calcium channel blockers such as diltiazem (Cardizem), nicardipine , nifedipine (Adalat, Procardia), and verapamil (Calan, Verelan, in Tarka); caspofungin (Cancidas); chloramphenicol; cimetidine (Tagamet); cisapride (Propulsid; not available in the U.S.); cisplatin ; danazol; certain diuretics (‘water pills’); ganciclovir (Valcyte); certain hormonal contraceptives (birth control pills, patches, rings, inserts, or injections); certain medications for HIV such as didanosine (Videx); indinavir (Crixivan), lamivudine (Epivir); nelfinavir (Viracept), ritonavir (Norvir), stavudine (Zerit), and zidovudine (Retrovir) lansoprazole (Prevacid); methylprednisolone (Medrol); metoclopramide (Reglan); mycophenolate (Cellcept); nefazodone; omeprazole (Prilosec); prednisone; rifabutin (Mycobutin); rifampin (Rifadin, Rimactane); certain medications for seizures such as carbamazepine (Tegretol, Teril), phenobarbital, and phenytoin (Dilantin, Phenytek);sirolimus (Rapamune), and telaprevir (Incivek; no longer available in U.S.). Your doctor may need to change the doses of your medications or monitor you more carefully for side effects. Many other medications may also interact with tacrolimus, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor if you are taking or have recently stopped taking cyclosporine (Gengraf, Neoral, Sandimmune). If you were taking cyclosporine, your doctor will probably tell you not to start taking tacrolimus until 24 hours after you took your last dose of cyclosporine. If you stop taking tacrolimus, your doctor will also tell you to wait 24 hours before starting to take cyclosporine.
- tell your doctor and pharmacist what herbal products you are taking, especially St. John’s wort or schisandra sphenanthera extracts. Do not take these herbal products while taking tacrolimus.
- tell your doctor if you have or have ever had QT syndrome (an inherited condition in which a person is more likely to have QT prolongation) low levels of potassium, calcium, or magnesium in your blood, an irregular heartbeat, high cholesterol levels, heart, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you or your partner are able to become pregnant, use effective birth control before and during treatment with tacrolimus. If you become pregnant while taking tacrolimus, call your doctor. Tacrolimus may harm the fetus.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking tacrolimus.
- you should know that taking tacrolimus may increase the risk that you will develop skin cancer. Protect yourself from skin cancer by avoiding unnecessary or prolonged exposure to sunlight or ultraviolet light (tanning beds) and wearing protective clothing, sunglasses, and sunscreen with a high skin protection factor (SPF).
- do not drink alcoholic beverages while you are taking tacrolimus extended-release capsules or extended-release tablets. Alcohol can make the side effects of tacrolimus worse.
- you should know that tacrolimus may cause high blood pressure. Your doctor will monitor your blood pressure carefully and may prescribe medication to treat high blood pressure if it develops.
- you should know that there is a risk that you will develop diabetes during your treatment with tacrolimus. African American and Hispanic patients who have had kidney transplants have an especially high risk of developing diabetes during their treatment with tacrolimus. Tell your doctor if you or anyone in your family has or has ever had diabetes. If you experience any of the following symptoms, call your doctor immediately: excessive thirst; excessive hunger; frequent urination; blurred vision, or confusion.
- do not have any vaccinations without talking to your doctor.
Dosage Of Tacrolimus
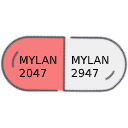
Tacrolimus comes as a capsule, granules for oral suspension (to be mixed with liquid), an extended-release (long-acting) capsule, and an extended-release tablet to take by mouth. The immediate-release capsules (Prograf) and oral suspension (Prograf) are usually taken twice a day (12 hours apart). You may take the immediate-release capsules and oral suspension either with or without food, but be sure to take it the same way each time. The extended-release capsules (Astagraf XL) or extended-release tablets (Envarsus XR) are usually taken every morning on an empty stomach at least 1 hour before or breakfast or at least 2 hours after breakfast. Take tacrolimus at the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take tacrolimus exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
If you are taking the granules for oral suspension, you will need to mix it with room temperature water before use. Place 1 to 2 tablespoons (15 to 30 milliliters) of water into a cup containing the granules. Mix the contents and then immediately take the mixture by mouth from the cup or with an oral syringe; do not save the mixture for a later time. The granules will not completely dissolve. If any of the mixtures remains, add 1 to 2 tablespoons (15 to 30 milliliters) of water to the mixture and immediately take it.
Swallow the extended-release capsules and extended-release tablets whole with water; do not split, chew, or crush them. Do not open the immediate-release capsules,
Your doctor will monitor you carefully and adjust your dose as needed. Talk to your doctor often about how you are feeling during your treatment. Ask your doctor if you have any questions about how much tacrolimus you should take.
Different tacrolimus products release the medication differently in your body and cannot be used interchangeably. Only take the tacrolimus product prescribed by your doctor and do not switch to a different tacrolimus product unless your doctor says that you should.
Tacrolimus can only prevent rejection of your transplant as long as you are taking the medication. Continue to take tacrolimus even if you feel well. Do not stop taking tacrolimus without talking to your doctor.
Other
Keep all appointments with your doctor and the laboratory. Your doctor will order certain tests before and during your treatment to check your body’s response to tacrolimus.
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.