Overview of Achilles Tendinopathy
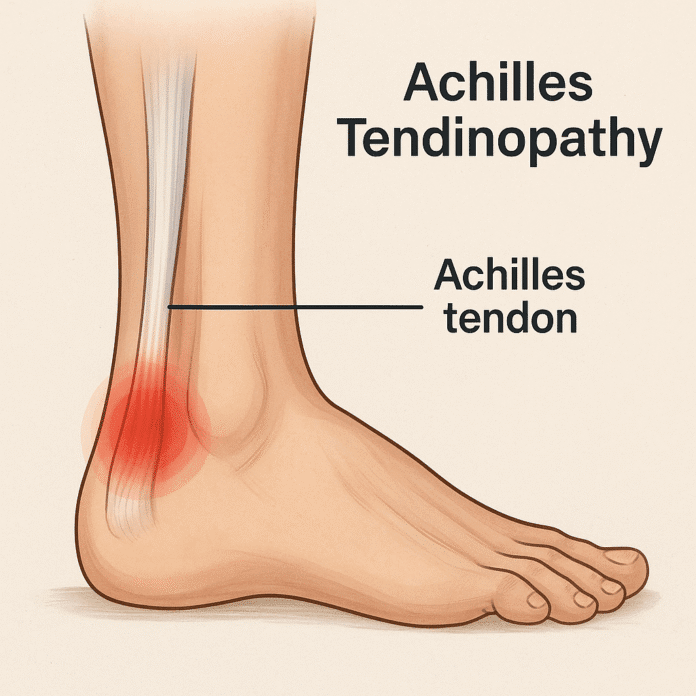
Achilles tendinopathy is a condition characterized by pain, stiffness, and impaired function of the Achilles tendon — the strong, fibrous tissue connecting the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). It is one of the most common overuse injuries in the lower limb, particularly among runners, athletes, and individuals engaged in repetitive physical activity. Achilles tendinopathy can be classified into two main types: insertional, which affects the tendon where it attaches to the heel bone, and non-insertional, which involves the middle portion of the tendon. Over time, microtears and degeneration can occur, leading to chronic pain and reduced tendon strength if left untreated.
Commonly Associated with Achilles Tendinopathy
Achilles tendinopathy is frequently seen in:
- Long-distance runners, sprinters, and jumpers
- Individuals with sudden increases in physical activity or training intensity
- Middle-aged recreational athletes (“weekend warriors”)
- People with flat feet (pes planus) or high arches (pes cavus)
- Those who wear improper footwear with inadequate heel support
- Patients with tight calf muscles, obesity, or metabolic disorders (such as diabetes)
It is also associated with certain systemic conditions like inflammatory arthritis and can be aggravated by the use of fluoroquinolone antibiotics or corticosteroids.
Causes of Achilles Tendinopathy
Achilles tendinopathy develops primarily due to overuse and repetitive stress that exceeds the tendon’s capacity for repair. Common contributing factors include:
- Sudden increase in training load, intensity, or duration
- Inadequate warm-up or stretching before physical activity
- Biomechanical abnormalities, such as overpronation or leg length discrepancies
- Improper footwear that fails to support the heel and arch
- Aging-related degeneration, as tendon elasticity decreases over time
- Intrinsic factors like poor vascular supply or genetic predisposition affecting tendon structure
These factors lead to microtrauma, collagen disorganization, and degeneration rather than acute inflammation, distinguishing tendinopathy from tendinitis.
Symptoms of Achilles Tendinopathy
Symptoms typically develop gradually and may include:
- Pain and stiffness in the Achilles tendon, especially in the morning or after rest
- Tenderness and swelling along the tendon or at its insertion near the heel
- Pain during or after exercise, which may improve during activity but worsen afterward
- Thickening of the tendon due to chronic degeneration
- Reduced strength and range of motion in the affected ankle
- A creaking or crackling sensation (crepitus) with tendon movement in some cases
Without treatment, pain can become persistent, significantly limiting daily activities and athletic performance.
Exams & Tests for Achilles Tendinopathy
Diagnosis is primarily clinical, based on history and physical examination. Key steps include:
- Palpation of the tendon to assess tenderness, swelling, and nodularity
- Range of motion and strength testing of the ankle and calf muscles
- Functional tests such as the single-leg heel raise to evaluate tendon capacity
Imaging studies may be used to confirm the diagnosis or rule out other conditions:
- Ultrasound: Reveals tendon thickening, hypoechoic areas, or neovascularization.
- MRI: Provides detailed visualization of tendon degeneration, partial tears, or associated bursitis.
Treatment of Achilles Tendinopathy
Management focuses on reducing pain, promoting tendon healing, and preventing recurrence. Treatment strategies include:
Conservative Management (first-line):
- Activity modification to reduce load on the tendon while maintaining fitness (e.g., swimming, cycling)
- Eccentric strengthening exercises to improve tendon resilience and stimulate collagen repair
- Stretching and physical therapy for calf muscles and Achilles tendon
- Orthotic devices or heel lifts to reduce tendon strain
- Ice therapy and nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief
Advanced and Adjunct Therapies:
- Extracorporeal shockwave therapy (ESWT) to stimulate healing in chronic cases
- Platelet-rich plasma (PRP) injections (evidence is still evolving)
- Surgical intervention for severe, refractory cases involving tendon debridement or repair
Early diagnosis and adherence to a structured rehabilitation program are key to optimal recovery and minimizing the risk of chronic tendon damage or rupture.
Source
- Maffulli N, Longo UG, Denaro V. “Achilles tendinopathy.” BMJ 2010; 340:c2469.
- Alfredson H, Cook J. “A treatment algorithm for managing Achilles tendinopathy: new treatment options.” Br J Sports Med 2007; 41(4):211–216.
- Khan KM, et al. “Time to abandon the ‘tendinitis’ myth.” BMJ 2002; 324(7338):626–627.
)