Overview of Acute Lymphoblastic Leukaemia in Children
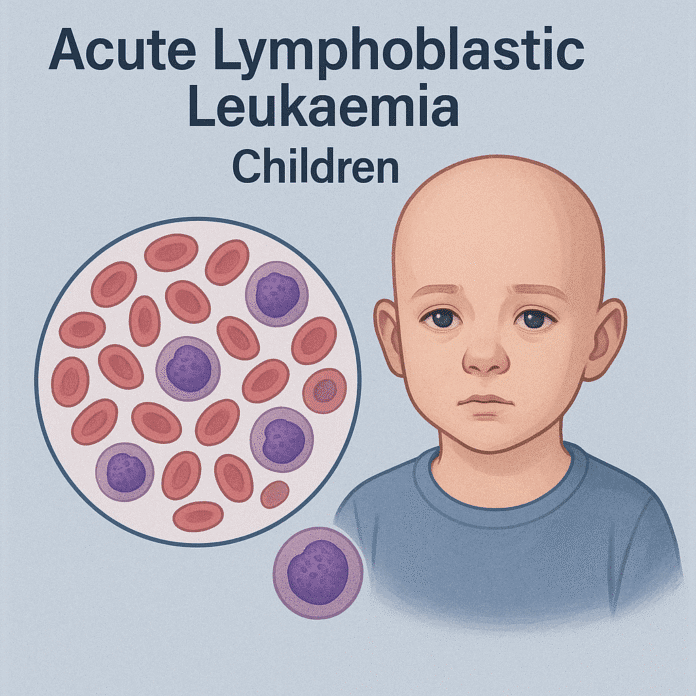
Acute lymphoblastic leukaemia (ALL) is the most common type of childhood cancer, accounting for about 75–80% of all childhood leukaemia cases. It is a fast-growing cancer of the blood and bone marrow caused by the abnormal proliferation of immature lymphoid cells, known as lymphoblasts. These malignant cells crowd out normal blood cell production, leading to anemia, frequent infections, and bleeding problems.
ALL most often occurs between the ages of 2 and 5 years and has a slightly higher incidence in boys. With early diagnosis and modern therapies, long-term remission is achieved in over 85–90% of pediatric patients, making ALL one of the most curable childhood cancers.
Commonly Associated with Acute Lymphoblastic Leukaemia in Children
Childhood ALL is associated with several genetic, environmental, and biological factors:
- Age and gender: Peak incidence between 2–5 years, more common in boys.
- Genetic syndromes: Down syndrome, Bloom syndrome, ataxia-telangiectasia, and Fanconi anemia increase risk.
- Family history: Siblings of children with ALL have a slightly higher risk.
- Previous cancer therapy: Chemotherapy or radiation for another cancer increases risk.
- Environmental exposures: High-dose ionizing radiation or exposure to certain chemicals (e.g., benzene).
- Chromosomal abnormalities: Philadelphia chromosome (t[9;22]) and MLL gene rearrangements are associated with certain subtypes.
Causes of Acute Lymphoblastic Leukaemia in Children
The precise cause of childhood ALL is not fully understood, but it is thought to arise from genetic mutations in immature lymphoid cells during early development. These mutations cause unchecked cell division and prevent normal lymphocytes from maturing. Potential contributing factors include:
- Chromosomal translocations (e.g., TEL-AML1, BCR-ABL) that activate oncogenes or deactivate tumor suppressor genes.
- Inherited genetic predispositions that impair DNA repair or immune regulation.
- Environmental exposures to radiation or chemicals during pregnancy or early childhood.
- Random DNA replication errors during normal immune cell development.
In most children, no single cause is identified, and the disease likely results from a combination of genetic susceptibility and environmental triggers.
Symptoms of Acute Lymphoblastic Leukaemia in Children
Symptoms of ALL in children usually develop rapidly over a few weeks as malignant lymphoblasts replace normal blood cells. Common signs and symptoms include:
- Anemia-related: Fatigue, pale skin, shortness of breath
- Low white blood cells: Frequent infections, fevers
- Low platelets: Easy bruising, nosebleeds, bleeding gums, petechiae
- Bone and joint pain: Caused by bone marrow expansion
- Swollen lymph nodes, liver, or spleen
- Loss of appetite, weight loss
- Fever and night sweats
- Neurological symptoms: Headaches, vomiting, vision changes if central nervous system involvement occurs
Parents may notice their child becoming unusually tired, irritable, or prone to infections and bruising.
Exams & Tests for Acute Lymphoblastic Leukaemia in Children
Diagnosis of childhood ALL involves a series of blood and bone marrow tests:
- Complete blood count (CBC): Often shows anemia, low platelets, and abnormal white blood cells.
- Peripheral blood smear: Reveals immature lymphoblasts.
- Bone marrow aspiration and biopsy: Confirms diagnosis with ≥20% lymphoblasts.
- Immunophenotyping (flow cytometry): Determines B-cell or T-cell origin.
- Cytogenetic and molecular tests: Detect chromosomal changes (e.g., BCR-ABL) important for prognosis.
- Lumbar puncture: Checks for leukemia cells in the cerebrospinal fluid.
- Imaging (e.g., chest X-ray): May reveal mediastinal masses, especially in T-cell ALL.
Treatment of Acute Lymphoblastic Leukaemia in Children
Treatment for childhood ALL is intensive but highly effective and follows a multi-phase approach:
1. Induction Therapy:
- Goal: Achieve remission within the first 4–6 weeks.
- Treatment: Combination chemotherapy (vincristine, corticosteroids, asparaginase, anthracyclines).
2. Consolidation (Intensification) Therapy:
- Goal: Eliminate residual disease and prevent relapse.
- Treatment: High-dose chemotherapy ± targeted therapies.
3. Maintenance Therapy:
- Goal: Prevent relapse over 2–3 years.
- Treatment: Low-dose oral chemotherapy (methotrexate, mercaptopurine).
4. Central Nervous System (CNS) Prophylaxis:
- Intrathecal chemotherapy and sometimes cranial irradiation to prevent CNS involvement.
5. Targeted and Immunotherapies:
- Tyrosine kinase inhibitors (e.g., imatinib) for Philadelphia chromosome-positive ALL.
- Monoclonal antibodies (e.g., blinatumomab) and CAR T-cell therapy in relapsed/refractory cases.
6. Stem Cell Transplantation:
- Considered for high-risk or relapsed patients.
Supportive care, including blood transfusions, infection prevention, and nutritional support, is crucial throughout treatment.
Source
- Hunger SP, Mullighan CG. “Acute lymphoblastic leukemia in children.” N Engl J Med 2015; 373(16):1541–1552.
- Pui C-H, et al. “Pediatric acute lymphoblastic leukemia: progress through collaboration.” J Clin Oncol 2021; 39(36):4126–4140.
- National Cancer Institute. “Childhood Acute Lymphoblastic Leukemia Treatment (PDQ®) – Health Professional Version.” NCI, 2024.