Overview of Acute Respiratory Infection (ARI)
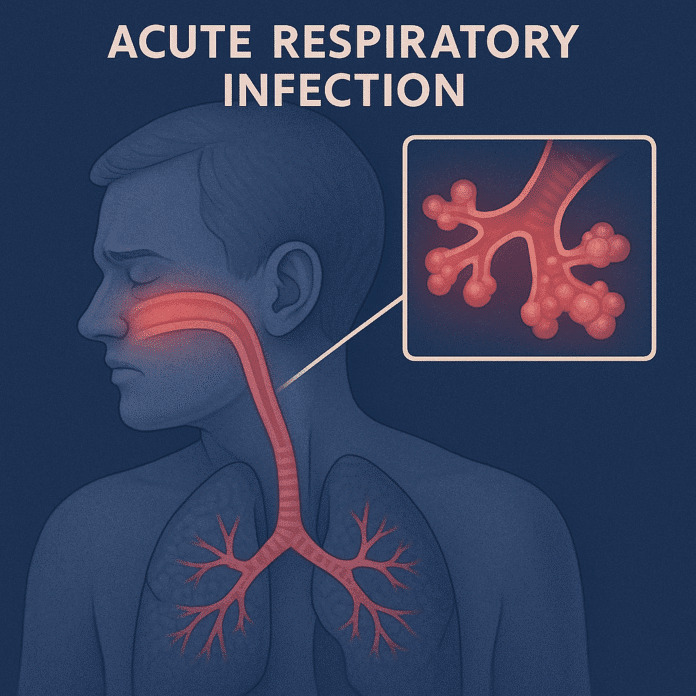
Acute respiratory infection (ARI) is a sudden infection that affects the respiratory system, including the nose, throat, airways, and lungs. It is one of the most common illnesses globally, responsible for significant morbidity and mortality, particularly among children under 5 years, the elderly, and immunocompromised individuals. ARIs range from mild infections such as the common cold and pharyngitis to severe illnesses like pneumonia and bronchiolitis.
These infections are primarily caused by viruses or bacteria and spread through droplets when an infected person coughs, sneezes, or talks. Most ARIs are self-limiting, but severe cases can progress quickly and require urgent medical attention.
Commonly Associated With Acute Respiratory Infection (ARI)
ARI is frequently linked to various factors, populations, and settings:
- Young children and infants – due to immature immune systems.
- Elderly individuals – higher susceptibility and risk of complications.
- Crowded environments – such as schools, daycare centers, and nursing homes.
- Weakened immunity – from HIV/AIDS, malnutrition, or chronic illnesses.
- Chronic respiratory conditions – including asthma and COPD.
- Environmental exposures – air pollution, tobacco smoke, and biomass fuel.
- Seasonal changes – incidence peaks during colder months.
- Unvaccinated individuals – particularly for influenza, pertussis, and pneumococcal disease.
Causes of Acute Respiratory Infection (ARI)
ARIs result from infection by a wide range of viruses, bacteria, and occasionally fungi. Pathogens enter the respiratory tract via inhaled droplets or contact with contaminated surfaces and trigger inflammation.
Viral causes:
- Influenza virus
- Respiratory syncytial virus (RSV)
- Rhinovirus
- Adenovirus
- Parainfluenza virus
- Coronavirus (including SARS-CoV-2)
Bacterial causes:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Mycoplasma pneumoniae
- Bordetella pertussis
- Staphylococcus aureus
Predisposing factors:
- Poor nutrition
- Inadequate immunization
- Exposure to pollutants
- Close contact with infected individuals
Symptoms of Acute Respiratory Infection (ARI)
The clinical presentation depends on whether the infection affects the upper respiratory tract (nose, throat, sinuses) or the lower respiratory tract (bronchi, bronchioles, lungs). Symptoms usually develop suddenly and may range from mild to severe.
Upper respiratory infection symptoms:
- Runny or congested nose
- Sore throat
- Sneezing and coughing
- Mild fever
- Headache and fatigue
Lower respiratory infection symptoms:
- Persistent or productive cough
- Shortness of breath or difficulty breathing
- Chest pain or tightness
- High fever and chills
- Wheezing or crackling sounds in the lungs
- Rapid or labored breathing (especially in infants and young children)
Severe cases can lead to pneumonia, acute respiratory distress, or respiratory failure.
Exams & Tests for Acute Respiratory Infection (ARI)
Diagnosis is based on clinical evaluation, laboratory testing, and imaging when necessary:
- Physical examination: Listening to lung sounds for wheezing, crackles, or decreased air entry.
- Complete blood count (CBC): May show elevated white blood cells in bacterial infections.
- Chest X-ray: Detects pneumonia, bronchitis, or other lung involvement.
- Pulse oximetry: Measures oxygen saturation levels.
- Sputum or throat culture: Identifies bacterial pathogens.
- Rapid antigen or PCR tests: Detect viruses like influenza, RSV, or SARS-CoV-2.
- Nasopharyngeal swabs: Commonly used to confirm viral causes.
Treatment of Acute Respiratory Infection (ARI)
Treatment depends on the cause, severity, and patient’s age or underlying health conditions. Most mild viral ARIs resolve spontaneously, while bacterial infections require specific therapy.
1. Supportive Care:
- Adequate rest and hydration.
- Pain and fever relief with acetaminophen or ibuprofen.
- Saline nasal sprays or steam inhalation to ease congestion.
- Humidified air to soothe airways.
2. Antiviral Therapy:
- Antiviral medications (e.g., oseltamivir) for influenza if started within 48 hours.
3. Antibiotics:
- Reserved for bacterial infections such as bacterial pneumonia or streptococcal pharyngitis.
- Avoid unnecessary use to prevent antibiotic resistance.
4. Hospital Care for Severe ARI:
- Oxygen therapy for hypoxia.
- Intravenous fluids and antibiotics if needed.
- Mechanical ventilation in severe respiratory failure.
5. Prevention:
- Vaccination – against influenza, pertussis, and pneumococcal disease.
- Good hygiene – regular handwashing and avoiding close contact with sick individuals.
- Avoiding tobacco smoke and air pollutants.
- Proper nutrition to support immunity.
Source
- WHO. “Acute respiratory infections (ARI): Fact sheet.” World Health Organization, 2023.
- Troeger C, et al. “Estimates of the global burden of acute respiratory infections in children.” Lancet Infect Dis 2018; 18(11):1191–1210.
- Jain S, et al. “Community-acquired pneumonia requiring hospitalization among U.S. children.” N Engl J Med 2015; 372(9):835–845.