Overview
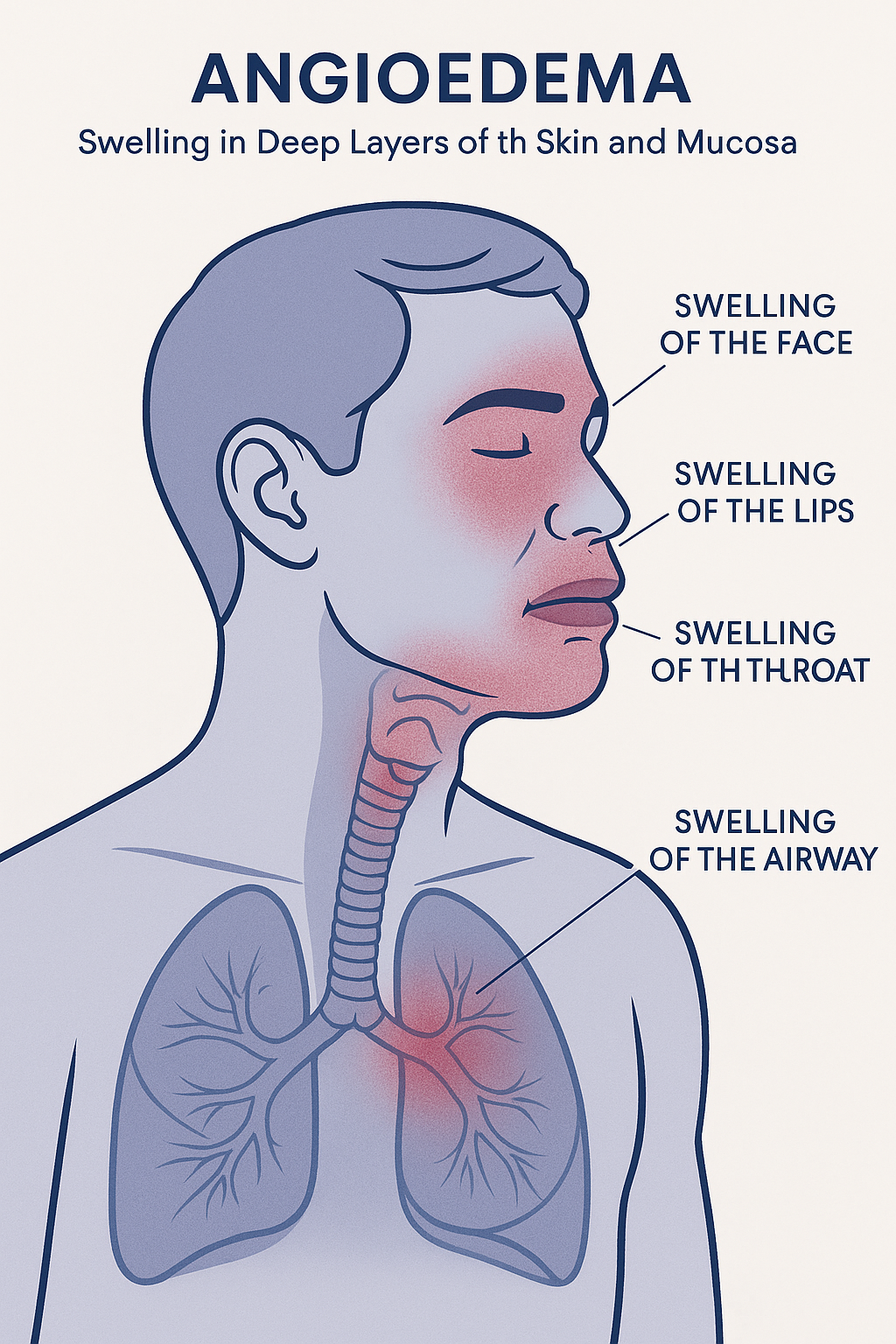
Angioedema is a sudden, localized swelling of the deeper layers of the skin and mucous membranes caused by increased vascular permeability. It most commonly affects areas such as the face, lips, tongue, throat, hands, feet, and genitals. While it is often self-limiting and resolves within 24–72 hours, it can be life-threatening when it involves the airway, leading to breathing difficulties.
It is closely related to urticaria (hives), but unlike urticaria — which affects the superficial skin — it involves deeper subcutaneous or submucosal tissues. It may occur in isolation or alongside hives and is often triggered by allergic reactions, medications, or hereditary factors.
Commonly Associated
Angioedema can occur due to various causes and is associated with the following conditions and risk factors:
- Allergic reactions: Food (e.g., nuts, shellfish), insect stings, latex, or medications.
- Medications: Especially ACE inhibitors (used for high blood pressure) and NSAIDs.
- Hereditary angioedema (HAE): A genetic deficiency or dysfunction of C1 esterase inhibitor.
- Acquired angioedema: Associated with autoimmune diseases or lymphoproliferative disorders.
- Idiopathic angioedema: No identifiable cause.
- Chronic urticaria: Angioedema often coexists with chronic hives in allergic conditions.
Causes of Angioedema
The underlying cause depends on its type and mechanism:
- Allergic (histamine-mediated) angioedema:
Triggered by allergens such as food, insect venom, or medications. Mast cell activation releases histamine, leading to increased vascular permeability and swelling.
- Drug-induced angioedema (e.g., ACE inhibitors):
Caused by accumulation of bradykinin, leading to vasodilation and fluid leakage into tissues. It is not related to histamine and does not respond to typical allergy medications.
- Hereditary angioedema (HAE):
A rare autosomal dominant disorder caused by deficiency or dysfunction of C1 esterase inhibitor, resulting in excessive bradykinin activity.
- Acquired angioedema:
Similar mechanism to HAE but develops later in life and is often secondary to underlying conditions.
Symptoms
Symptoms usually appear suddenly and develop over minutes to hours. They may last from 24 to 72 hours, depending on the cause.
Common signs and symptoms include:
- Swelling of the skin and mucous membranes, often around the eyes, lips, cheeks, or genitals.
- Swelling of the tongue, throat, or larynx, potentially causing difficulty breathing, swallowing, or speaking — a medical emergency.
- Abdominal pain, nausea, or vomiting – in cases involving gastrointestinal mucosa.
- Tingling, burning, or warmth in affected areas (pain is less common).
- No itching – unlike hives, it typically does not itch.
- Urticaria (hives): May accompany histamine-mediated angioedema.
Warning signs of severe angioedema (anaphylaxis-related):
- Rapid swelling of tongue or throat
- Hoarse voice or stridor
- Shortness of breath or wheezing
- Dizziness or fainting due to low blood pressure
Exams & Tests
Diagnosis is primarily clinical, based on history and physical examination. Additional tests help identify the cause and type:
- Medical history: Exposure to allergens, medications, or family history.
- Physical examination: Assessment of swelling location, severity, and airway involvement.
- Blood tests:
- C4 complement and C1 esterase inhibitor levels – to diagnose hereditary or acquired angioedema.
- Tryptase levels – elevated in allergic (mast cell–mediated) angioedema.
- Allergy testing: Skin prick or specific IgE blood tests if an allergic cause is suspected.
- Genetic testing: Confirm hereditary angioedema in suspected cases.
Treatment
Treatment depends on the underlying cause and severity. Immediate intervention is critical if airway compromise is suspected.
1. Emergency Management (Airway Protection):
- Epinephrine (adrenaline): Intramuscular injection in cases of anaphylaxis.
- Airway support: Intubation or tracheostomy if swelling threatens the airway.
- Oxygen and IV fluids: For patients in shock or with severe symptoms.
2. Pharmacological Management (Histamine-Mediated):
- Antihistamines: Reduce swelling and allergic response.
- Corticosteroids: Decrease inflammation and prevent recurrence.
- Beta-agonists (e.g., albuterol): For associated bronchospasm.
3. Treatment of Bradykinin-Mediated Angioedema (e.g., ACE inhibitor-induced, HAE):
- Discontinuation of ACE inhibitors immediately.
- C1 esterase inhibitor (C1-INH) concentrate: Replaces deficient enzyme in HAE.
- Icatibant: A bradykinin B2 receptor antagonist that rapidly reduces swelling.
- Ecallantide: A kallikrein inhibitor that reduces bradykinin production.
- Fresh frozen plasma (FFP): In emergency settings where specific treatments are unavailable.
4. Long-Term Management (for HAE):
- Prophylactic C1-INH replacement therapy or lanadelumab to prevent recurrent attacks.
- Avoiding known triggers (e.g., trauma, infections, certain medications).
Source
- Bernstein JA, et al. “International consensus on hereditary and acquired angioedema.” Allergy 2021; 76(5):1185–1199.
- Kaplan AP. “Angioedema.” N Engl J Med 2017; 377(4):393–394.
- Longhurst HJ, et al. “Hereditary angioedema: pathophysiology and treatment.” Clin Exp Allergy 2020; 50(4):420–430.