Overview
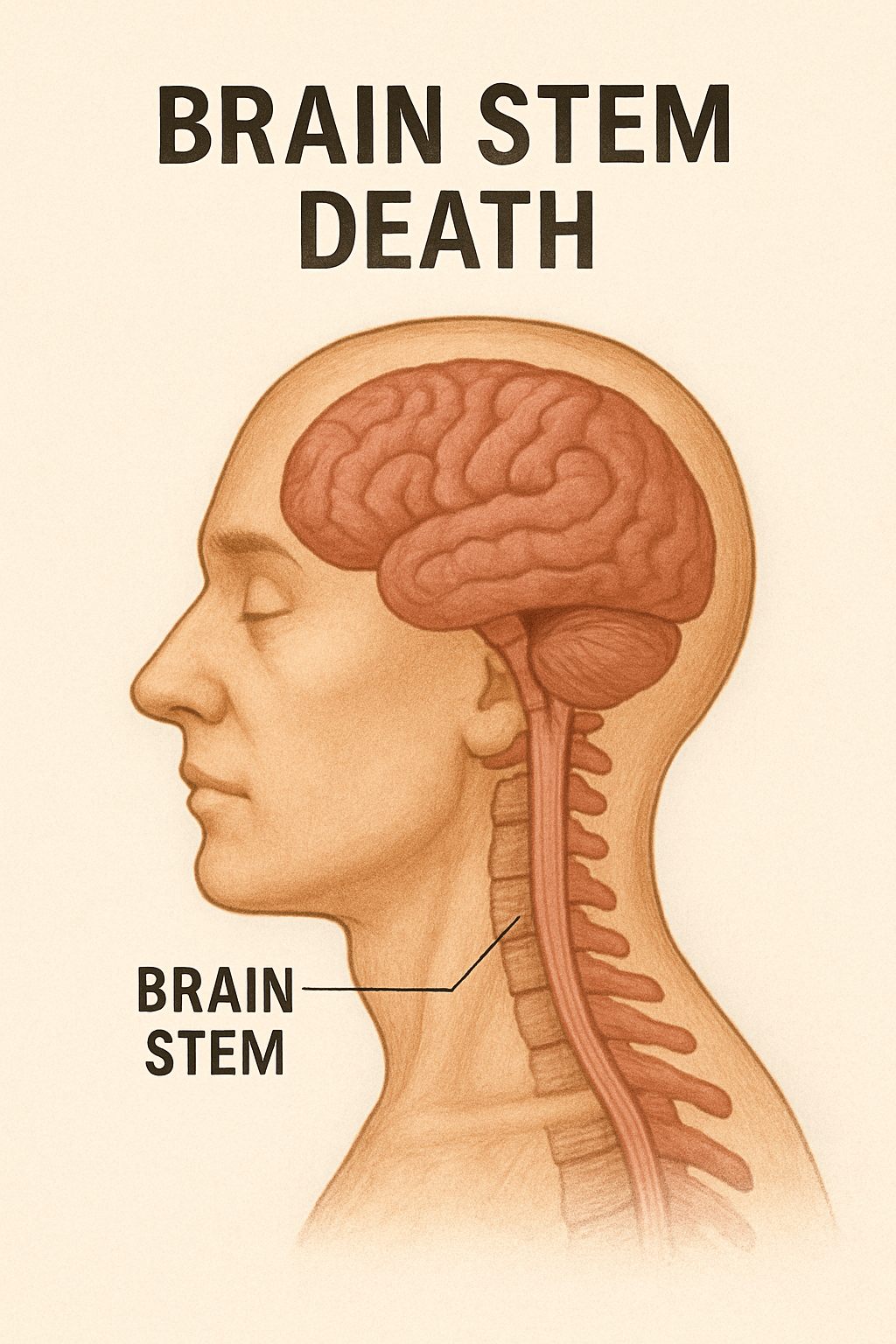
Brain stem death is the irreversible loss of all brain stem functions, including the ability to breathe, regulate vital reflexes, and maintain consciousness. The brain stem connects the brain to the spinal cord and controls essential life-sustaining activities such as breathing, heartbeat, and consciousness. When the brain stem ceases to function permanently, the individual is legally and clinically declared dead, even if a ventilator maintains the heartbeat and breathing artificially.
This diagnosis is crucial in critical care settings, particularly for decisions about life support withdrawal and organ donation.
Commonly Associated
Other terms and related conditions include:
- Brain death
- Brainstem death (alternate spelling)
- Irreversible cessation of brain function
- Neurological death
Causes
Brain stem death occurs due to severe and irreversible damage to the brain. Common causes include:
- Severe traumatic brain injury – Major head trauma causing swelling and irreversible damage.
- Stroke – Massive hemorrhagic or ischemic stroke affecting the brain stem.
- Prolonged cardiac arrest – Extended loss of oxygen to the brain (hypoxic-ischemic injury).
- Brain hemorrhage – Intracerebral or subarachnoid bleeding leading to brain swelling and herniation.
- Brain infections – Severe meningitis or encephalitis causing widespread brain injury.
- Brain tumors – Rapidly growing or untreated tumors compressing the brain stem.
- Complications from neurosurgery or anesthesia – Rare but possible causes.
Symptoms
Brain stem death is characterized by the complete and irreversible absence of all brain stem functions, including:
- No response to external stimuli – Deep coma with no reaction to pain.
- No brain stem reflexes – Loss of pupil reaction to light, corneal reflex, and gag reflex.
- Absence of spontaneous breathing – Patient cannot breathe independently without a ventilator.
- Fixed, dilated pupils – Indicative of loss of brain stem control.
- No eye movement – Eyes do not move when the head is turned (absent oculocephalic reflex).
Patients with brain stem death are in a deep, irreversible coma and require mechanical ventilation to sustain circulation.
Exams & Tests
A diagnosis of brain stem death is made through strict clinical criteria and multiple confirmatory tests, usually performed by two senior physicians:
- Clinical brain stem reflex tests – Check for absence of pupil response, corneal reflex, vestibulo-ocular reflex, and cough/gag reflex.
- Apnea test – Determines the absence of spontaneous breathing when carbon dioxide levels rise.
- Electroencephalogram (EEG) – May show no electrical activity, though not always required.
- Cerebral blood flow studies – Demonstrate absence of blood flow to the brain.
- Imaging (CT/MRI) – Can show severe brain injury or swelling but are supportive, not diagnostic.
The tests must confirm irreversible loss of function, and reversible causes such as hypothermia, drug intoxication, or metabolic disturbances must be excluded.
Treatment
There is no treatment for brain stem death, as the damage is irreversible. Once confirmed, the individual is legally declared dead. Management then focuses on:
- Withdrawal of life support – As the patient cannot sustain life independently.
- Organ donation – Organs may be maintained temporarily on ventilatory support for transplantation if consent is given.
- Family support and counseling – Compassionate communication with family members is essential to explain the diagnosis and next steps.
Source of Brain Stem Death
- National Health Service (NHS) – Brain Stem Death
- Mayo Clinic – Brain Death Overview
- American Academy of Neurology – Guidelines for Brain Death Determination