Uses of Apixaban
Apixaban is used help prevent strokes or blood clots in people who have atrial fibrillation (a condition in which the heart beats irregularly, increasing the chance of clots forming in the body and possibly causing strokes) that is not caused by heart valve disease. Apixaban is also used to prevent deep vein thrombosis (DVT; a blood clot, usually in the leg) and pulmonary embolism (PE; a blood clot in the lung) in people who are having hip replacement or knee replacement surgery. Apixaban is also used to treat DVT and PE and may be continued to prevent DVT and PE from happening again after the initial treatment is completed. Apixaban is in a class of medications called factor Xa inhibitors. It works by blocking the action of a certain natural substance that helps blood clots to form.
Side Effects of Apixaban
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately or get emergency medical treatment:
- bleeding gums
- nosebleeds
- heavy vaginal bleeding
- red, pink, or brown urine
- red or black, tarry stools
- coughing up or vomiting blood or material that looks like coffee grounds
- swelling or joint pain
- headache
- rash
- chest pain or tightness
- swelling of the face or tongue
- trouble breathing
- wheezing
- feeling dizzy or faint
Apixaban prevents blood from clotting normally, so it may take longer than usual for you to stop bleeding if you are cut or injured. This medication may also cause you to bruise or bleed more easily. Call your doctor right away if bleeding or bruising is unusual, severe, or cannot be controlled.
Apixaban may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Warnings & Precautions
Before taking apixaban:
- tell your doctor and pharmacist if you are allergic to apixaban, any other medications, or any of the ingredients in apixaban tablets. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Be sure to mention any of the following: carbamazepine (Carbatrol, Epitol, Equetro, Tegretol, Teril); clarithromycin (Biaxin, in Prevpac); itraconazole (Onmel, Sporanox); ketoconazole (Nizoral); phenytoin (Dilantin, Phenytek); rifampin (Rifadin, Rimactane, in Rifadin, in Rifater); ritonavir (Norvir, in Kaletra); selective serotonin reuptake inhibitors (SSRIs) such as citalopram (Celexa), fluoxetine (Prozac, Sarafem, Selfemra, in Symbyax), fluvoxamine (Luvox), paroxetine (Brisdelle, Paxil, Pexeva), and sertraline (Zoloft); and serotonin and norepinephrine reuptake inhibitors (SNRIs) such as duloxetine (Cymbalta), desvenlafaxine (Khedezla, Pristiq), milnacipran (Fetzima, Savella), and venlafaxine (Effexor). Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Many other medications may also interact with apixaban, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor what herbal products you are taking, especially St. John’s wort.
- you should know that apixaban may interact with certain medications that may be used to treat you if you have a stroke or other medical emergency. In case of an emergency, you or a family member should tell the doctor or emergency room staff who treat you that you are taking apixaban.
- tell your doctor if you have an artificial heart valve or if you have heavy bleeding anywhere in your body that cannot be stopped. Your doctor will probably tell you not to take apixaban.
- tell your doctor if you have or have ever had any type of bleeding problem, antiphospholipid syndrome (APS; a condition that causes blood clots), or kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking apixaban, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking apixaban. Your doctor may tell you to stop taking apixaban before the surgery or procedure. If you need to stop taking apixaban because you are having surgery, your doctor may prescribe a different medication to prevent blood clots during this time. Your doctor will tell you when you should start taking apixaban again after your surgery. Follow these directions carefully.
- Call your doctor right away if you fall or injure yourself, especially if you hit your head. Your doctor may need to check you.
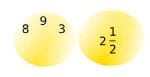
Dosage
Apixaban comes as a tablet to take by mouth. It is usually taken with or without food twice a day. When apixaban is taken to prevent DVT and PE after hip or knee replacement surgery, the first dose should be taken at least 12 to 24 hours after surgery. Apixaban is usually taken for 35 days after a hip replacement surgery and for 12 days after knee replacement surgery. Take apixaban at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take apixaban exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
If you are unable to swallow the tablets, you can crush them and mix with water, apple juice, or applesauce. Swallow the mixture right after you prepare it. Apixaban can also be given in certain types of feeding tubes. Ask your doctor if you should take this medication in your feeding tube. Follow your doctor’s directions carefully.
Continue to take apixaban even if you feel well. Do not stop taking apixaban without talking to your doctor. If you stop taking apixaban, your risk of a blood clot may increase.
Other
Keep all appointments with your doctor.
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.