Overview of Alzheimer’s Disease
Alzheimer’s disease is a progressive, irreversible neurodegenerative disorder that affects the brain’s memory, thinking, and behavior. It is the most common cause of dementia, accounting for about 60–80% of all cases, and primarily affects older adults, usually over the age of 65. Alzheimer’s disease develops slowly, beginning with mild memory loss and confusion and progressing to severe cognitive impairment and loss of independence.
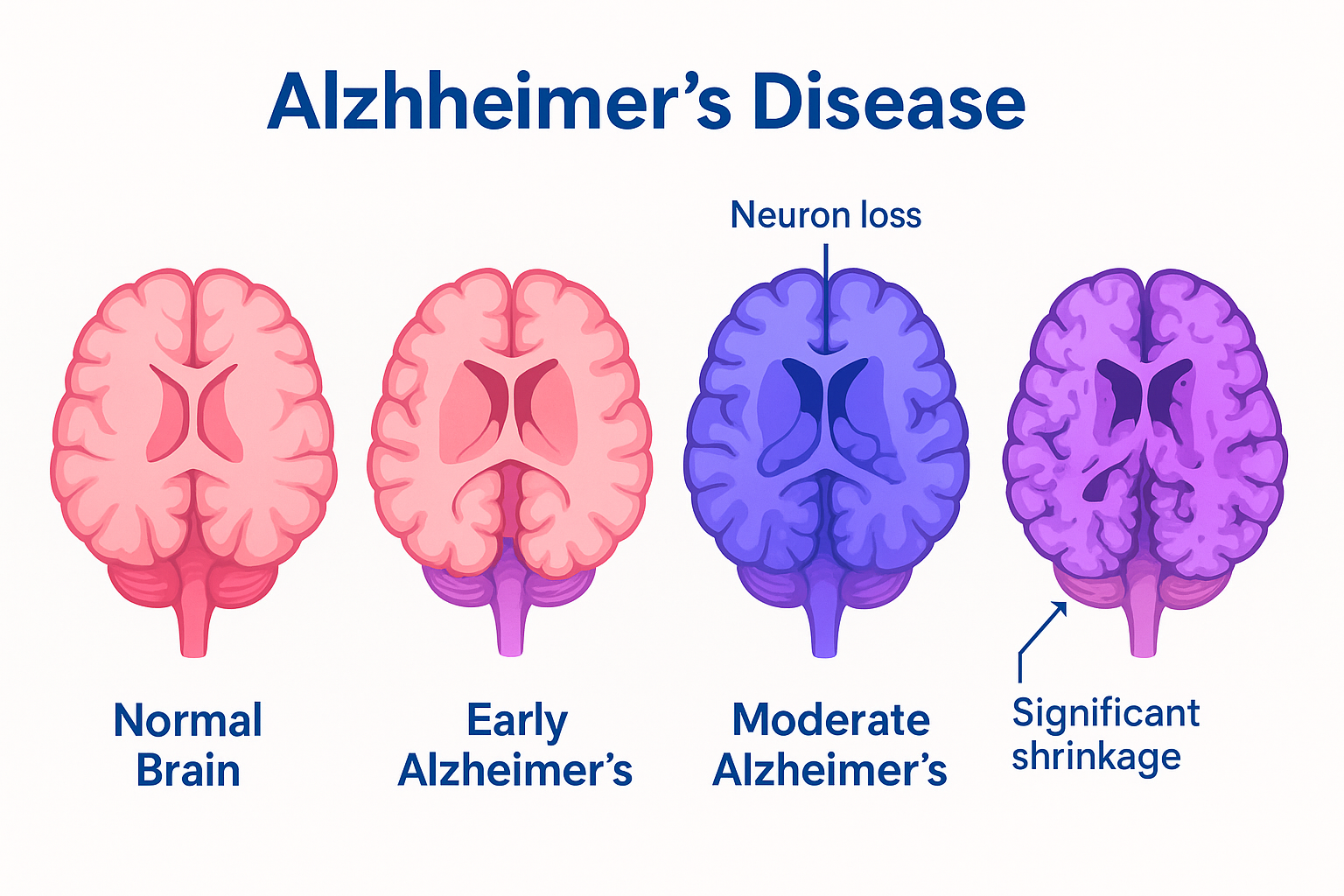
The disease is characterized by abnormal protein accumulations in the brain — beta-amyloid plaques outside neurons and tau tangles inside neurons — which disrupt communication between brain cells, leading to cell death and brain shrinkage. While there is currently no cure, early diagnosis and treatment can help manage symptoms and slow progression.
Commonly Associated with Alzheimer’s Disease
Several risk factors and conditions are strongly associated with Alzheimer’s disease:
- Advanced age – risk increases significantly after 65.
- Family history – especially first-degree relatives with Alzheimer’s.
- Genetic factors – such as the APOE ε4 allele, which increases susceptibility.
- Down syndrome – linked to an increased risk due to extra amyloid precursor protein production.
- Cardiovascular disease – hypertension, diabetes, obesity, and high cholesterol raise risk.
- Head trauma – severe or repeated head injuries.
- Lifestyle factors – low physical activity, poor diet, smoking, and social isolation.
- Low educational attainment and limited cognitive stimulation.
Causes of Alzheimer’s Disease
The exact cause of Alzheimer’s disease is not fully understood, but it is believed to result from a combination of genetic, environmental, and lifestyle factors that affect the brain over time. Key pathological features include:
- Beta-amyloid plaques: Sticky protein fragments accumulate between neurons, disrupting cell communication and triggering inflammation.
- Tau tangles: Abnormal tau proteins inside neurons form twisted tangles, impairing nutrient transport and leading to cell death.
- Neuroinflammation: Chronic brain inflammation exacerbates neuronal damage.
- Neurotransmitter deficiency: Decline in acetylcholine, crucial for memory and learning.
- Genetic mutations: Rare inherited mutations in APP, PSEN1, or PSEN2 genes cause early-onset Alzheimer’s.
The disease often develops decades before symptoms appear, beginning with subtle changes in brain structure and chemistry.
Symptoms of Alzheimer’s Disease
Alzheimer’s disease progresses gradually and is typically divided into three stages: early, moderate, and severe. Symptoms worsen over time as brain cells are progressively damaged and destroyed.
Early stage (mild):
- Memory lapses (forgetting recent events or conversations)
- Difficulty finding words
- Misplacing items
- Trouble planning or organizing
- Subtle personality or mood changes
Middle stage (moderate):
- Increased memory loss and confusion
- Difficulty recognizing family and friends
- Problems with language and communication
- Wandering or getting lost
- Behavioral changes — agitation, aggression, depression
- Trouble with daily activities (dressing, cooking, managing finances)
Late stage (severe):
- Inability to communicate coherently
- Severe memory loss
- Loss of awareness of surroundings
- Dependence on others for care
- Loss of bladder and bowel control
- Difficulty swallowing and increased risk of infections (e.g., pneumonia)
Exams & Tests for Alzheimer’s Disease
There is no single test for Alzheimer’s disease; diagnosis relies on a combination of clinical evaluation, cognitive testing, imaging, and laboratory studies.
- Medical history and neurological examination: Review of symptoms, family history, and physical signs.
- Cognitive assessments: Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), or other neuropsychological tests.
- Laboratory tests: Rule out reversible causes of dementia (e.g., thyroid dysfunction, vitamin B12 deficiency).
- Brain imaging:
- MRI or CT scan: Identify brain atrophy and exclude other conditions.
- PET scans: Detect amyloid or tau deposits and assess brain metabolism.
- Cerebrospinal fluid (CSF) analysis: Measures beta-amyloid and tau protein levels.
- Genetic testing: May identify inherited mutations in early-onset cases.
Early diagnosis allows for timely intervention, symptom management, and planning for future care.
Treatment of Alzheimer’s Disease
While there is currently no cure for Alzheimer’s disease, treatments aim to slow progression, manage symptoms, and improve quality of life.
1. Medications:
- Cholinesterase inhibitors (donepezil, rivastigmine, galantamine): Improve communication between nerve cells and manage cognitive symptoms.
- NMDA receptor antagonist (memantine): Helps regulate glutamate activity, improving memory and learning in moderate to severe disease.
- Disease-modifying therapies: Newer monoclonal antibodies (e.g., aducanumab, lecanemab) target beta-amyloid to slow disease progression in early stages.
2. Supportive Therapies:
- Cognitive stimulation therapy: Enhances memory and problem-solving skills.
- Behavioral and psychological interventions: Manage agitation, depression, and anxiety.
- Occupational therapy: Helps maintain independence in daily activities.
3. Lifestyle Modifications:
- Regular physical exercise to support brain and cardiovascular health.
- Healthy diet (e.g., Mediterranean diet) rich in antioxidants.
- Social engagement and mental stimulation to support cognitive function.
- Managing cardiovascular risk factors such as diabetes, hypertension, and high cholesterol.
4. Support for Caregivers:
- Education, counseling, and respite care are essential for those providing long-term support.
Source
- Alzheimer’s Association. “2024 Alzheimer’s Disease Facts and Figures.” Alzheimers Dement 2024; 20(3):501–610.
- Lane CA, Hardy J, Schott JM. “Alzheimer’s disease.” Eur J Neurol 2018; 25(1):59–70.
- Jack CR Jr., et al. “NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease.” Alzheimers Dement 2018; 14(4):535–562.