Uses
Lofexidine is used to manage opioid withdrawal symptoms (e.g., sick feeling, stomach cramps, muscle spasms or twitching, cold sensation, heart-pounding, muscle tension, aches and pains, yawning, runny eyes, or difficulty falling asleep or staying asleep) that may occur after an opioid medication is suddenly stopped. Lofexidine is in a class of medications called central alpha adrenergic agonists. It works by relaxing blood vessels so that blood can flow more easily through the body.
Side Effects Of Lofexidine
Lofexidine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- difficulty falling asleep or staying asleep
- dry mouth
- ringing in the ears
Some side effects can be serious. If you experience any of these symptoms or those listed in the WARNINGS AND PRECAUTIONS section, call your doctor immediately or get emergency medical treatment:
- fainting
- dizziness or lightheadedness
Lofexidine may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Warnings & Precautions
Before taking lofexidine:
- tell your doctor and pharmacist if you are allergic to lofexidine, any other medications, or any of the ingredients in lofexidine tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: amitriptyline; antidepressants; antifungals such as ketoconazole, itraconazole (Onmel, Sporanox), or voriconazole (Vfend); medications for anxiety; barbiturates such as phenobarbital (Luminal); benzodiazepines such as alprazolam (Xanax), lorazepam (Ativan), and triazolam (Halcion); clarithromycin (Biaxin, in Prevpac); erythromycin (E.E.S., E-Mycin, Erythrocin); granisetron (Kytril); haloperidol (Haldol); medications for high blood pressure; certain medications for human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS) such as atazanavir (Reyataz), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), and saquinavir (Invirase); certain medications for irregular heartbeat such as amiodarone (Pacerone), disopyramide (Norpace), dofetilide (Tikosyn), procainamide, quinidine, and sotalol (Betapace, Betapace AF, Sotylize); medications for mental illness; methadone (Dolophine, Methadose); naltrexone (Vivitrol) when given by mouth; ondansetron (Zofran); pain medications; paroxetine (Brisdelle, Paxil, Pexeva); sedatives; sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you or anyone in your family has or has ever had long QT syndrome (a condition that increases the risk of developing an irregular heartbeat that may cause fainting or sudden death), or another type of irregular heartbeat or heart rhythm problem, or if you have or have ever had low blood levels of magnesium or potassium in your blood, a heart attack, heart failure, low or high blood pressure, cerebrovascular disease (clogging or weakening of the blood vessels within the brain or leading to the brain), or heart, liver, or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking lofexidine, call your doctor.
- you should know that lofexidine may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- ask your doctor about the safe use of alcoholic beverages while you are taking lofexidine. Alcohol can make the side effects of lofexidine worse.
- you should know that lofexidine may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up. If you experience these symptoms, sit or lie down. If these symptoms do not improve, call your doctor.
- you should know that you may faint if you become dehydrated or overheated during your treatment with lofexidine. Be sure to drink plenty of liquids and stay cool while you are taking this medication.
- you should know that after a period of not using opioid drugs, you may be more sensitive to the effects of opioids and are at a greater risk of overdosing if you were to take or use too much.
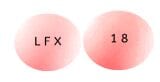
Lofexidine Dosage
Lofexidine comes as a tablet to take by mouth. It is usually taken with or without food four times a day (5 to 6 hours between each dose) to manage withdrawal symptoms after your last use of opioid medication. It may be taken for up to 14 days depending on your symptoms and side effects. Take lofexidine at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take lofexidine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may need to reduce, interrupt, or discontinue your treatment if you experience certain side effects. Talk to your doctor about how you are feeling during your treatment.
Lofexidine helps to reduce the severity of opioid withdrawal symptoms but may not completely prevent them. Do not stop taking lofexidine without talking to your doctor. If you suddenly stop taking lofexidine, your blood pressure may increase or you may experience withdrawal symptoms such as diarrhea, difficulty falling asleep or staying asleep, anxiety, chills, sweating, and leg or arm pain. Your doctor will probably tell you to decrease your dose gradually over 2 to 4 days.
Ask your pharmacist or doctor for a copy of the manufacturer’s information for the patient.
Other
Keep all appointments with your doctor. Your doctor may order certain lab tests to check your body’s response to lofexidine.
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.