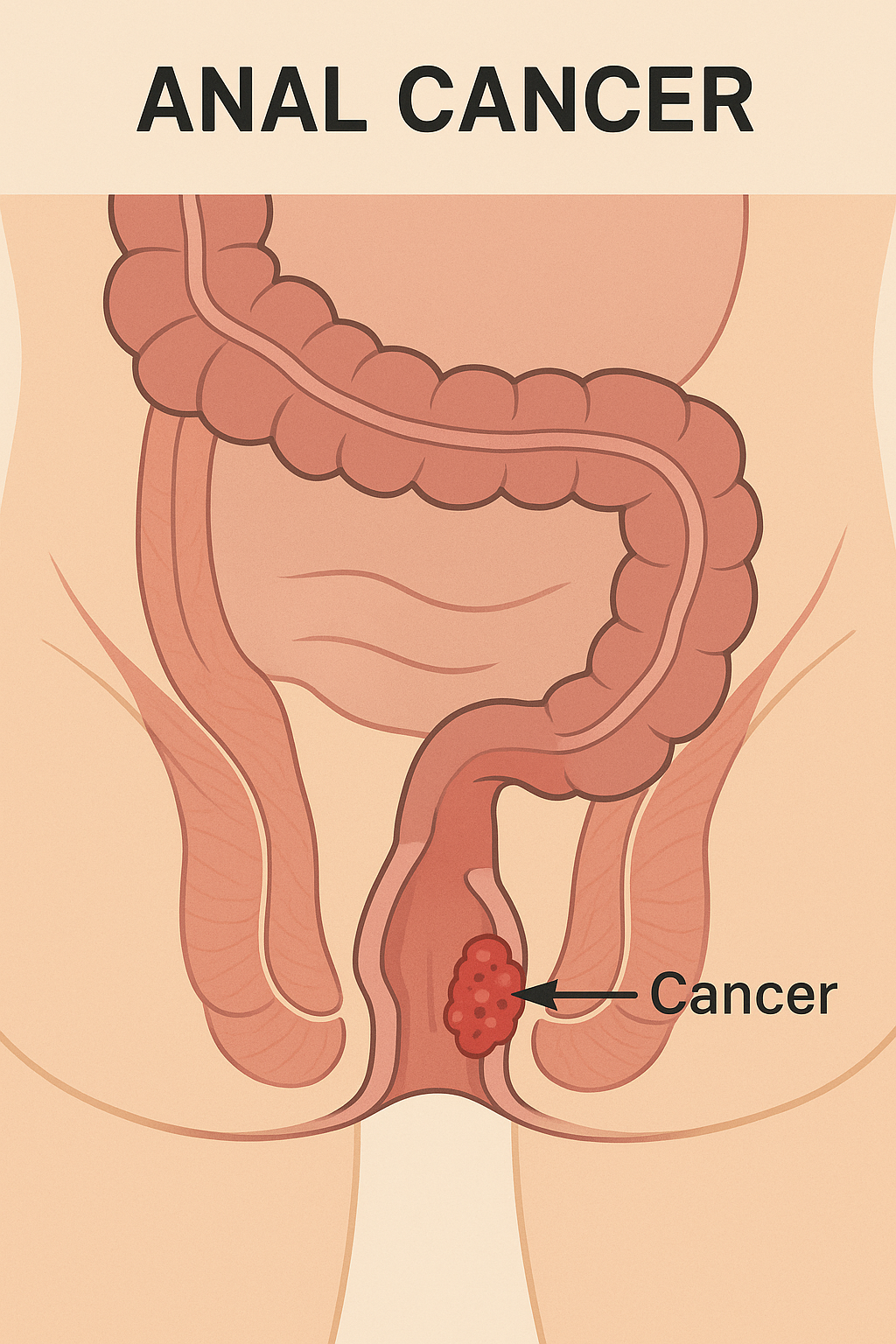
Overview of Anal Cancer
Anal cancer is a malignant growth that develops in the anal canal, the short passage at the end of the rectum through which stool exits the body. It is a relatively rare cancer, accounting for about 2–4% of all gastrointestinal cancers, but its incidence has been rising in recent decades. Most cases are squamous cell carcinomas, originating from the epithelial cells lining the anal canal.
Anal cancer often develops slowly and may initially cause subtle symptoms, leading to delayed diagnosis. It is strongly associated with human papillomavirus (HPV) infection, and early detection greatly improves the chance of successful treatment. With advances in combined chemoradiation therapy, many patients achieve excellent long-term outcomes without requiring major surgery.
Commonly Associated with Anal Cancer
Several risk factors and conditions are linked to an increased risk of developing anal cancer:
- Human papillomavirus (HPV) infection – present in over 85% of cases.
- Anal intercourse – increases risk of HPV transmission.
- Human immunodeficiency virus (HIV) infection – impairs immune surveillance.
- Immunosuppression – due to organ transplantation or chronic conditions.
- History of cervical, vulvar, or vaginal cancer – linked to HPV-related disease.
- Chronic anal irritation or inflammation – from fistulas, fissures, or long-term infections.
- Smoking – increases risk of squamous cell carcinoma.
- Age and sex – most common in adults over 50, slightly more frequent in women.
Causes of Anal Cancer
The primary cause of anal cancer is persistent infection with high-risk HPV types, particularly HPV-16 and HPV-18, which trigger genetic changes in anal epithelial cells. These changes cause uncontrolled cell division and malignant transformation.
Other contributing factors include:
- Chronic inflammation or trauma – promotes abnormal cell growth.
- Immunosuppression – reduces the body’s ability to eliminate abnormal cells.
- Tobacco carcinogens – cause DNA damage and promote tumor growth.
- Co-infection with HIV – increases susceptibility to HPV persistence and malignancy.
Symptoms of Anal Cancer
Anal cancer may initially cause mild, nonspecific symptoms, which are often mistaken for benign conditions such as hemorrhoids. As the tumor grows, symptoms become more apparent:
- Rectal bleeding – the most common early sign.
- Pain or pressure in the anal area.
- Anal itching or irritation.
- A palpable lump or mass near the anus.
- Change in bowel habits – such as constipation or narrower stools.
- Mucous discharge from the anus.
- Swollen lymph nodes in the groin or anal region.
- In advanced stages: weight loss, fatigue, or pelvic pain.
Any persistent anal symptoms, particularly bleeding or lumps, should prompt medical evaluation.
Exams & Tests for Anal Cancer
Diagnosis involves a combination of clinical examination, imaging, and biopsy to confirm malignancy and assess disease extent:
- Digital rectal examination (DRE): Detects masses, tenderness, or irregularities in the anal canal.
- Anoscopy or proctoscopy: Direct visualization of the anal canal and rectum.
- Biopsy: Confirms the diagnosis and identifies cancer type.
- HPV testing: Determines the presence of high-risk HPV strains.
Imaging studies (to stage the disease):
- MRI of the pelvis: Assesses tumor depth and local spread.
- CT scan or PET-CT: Detects lymph node involvement or distant metastases.
- Endoanal ultrasound: Evaluates tumor invasion into surrounding tissues.
Staging follows the TNM system, considering tumor size (T), lymph node involvement (N), and metastasis (M).
Treatment of Anal Cancer
Treatment depends on the stage, size, and spread of the tumor, but most patients are treated effectively without requiring removal of the anus.
1. Combined Chemoradiation Therapy (Standard of Care):
- Combination of radiation therapy and chemotherapy (usually 5-fluorouracil and mitomycin C) is the mainstay treatment.
- Highly effective for early- and mid-stage disease, with cure rates exceeding 80–90%.
- Preserves anal function, avoiding the need for permanent colostomy in most cases.
2. Surgery:
- Local excision: For small, well-defined early-stage tumors.
- Abdominoperineal resection (APR): In advanced or recurrent disease, removal of the anus, rectum, and part of the colon with creation of a permanent colostomy.
3. Targeted and Immunotherapies:
- Immune checkpoint inhibitors (e.g., nivolumab, pembrolizumab) are used in advanced or metastatic cases.
4. Supportive Care:
- Pain relief, management of bowel function, and treatment of radiation-related side effects.
- Psychological support and rehabilitation services.
Prevention:
- HPV vaccination significantly reduces the risk of anal and other HPV-related cancers.
- Safe sexual practices and regular screening in high-risk populations.
Source
- National Comprehensive Cancer Network (NCCN). “Anal Carcinoma: Clinical Practice Guidelines in Oncology.” Version 1.2024.
- Glynne-Jones R, et al. “Anal cancer: ESMO Clinical Practice Guidelines.” Ann Oncol 2022; 33(7):675–687.
- Deshmukh AA, et al. “Anal cancer incidence trends and the impact of HPV vaccination.” J Natl Cancer Inst 2020; 112(10):994–1001.