Overview Of Immune Thrombocytopenic Purpura
Immune thrombocytopenic purpura (ITP) is a bleeding disorder in which the immune system destroys platelets, which are necessary for normal blood clotting. People with the disease have too few platelets in the blood.
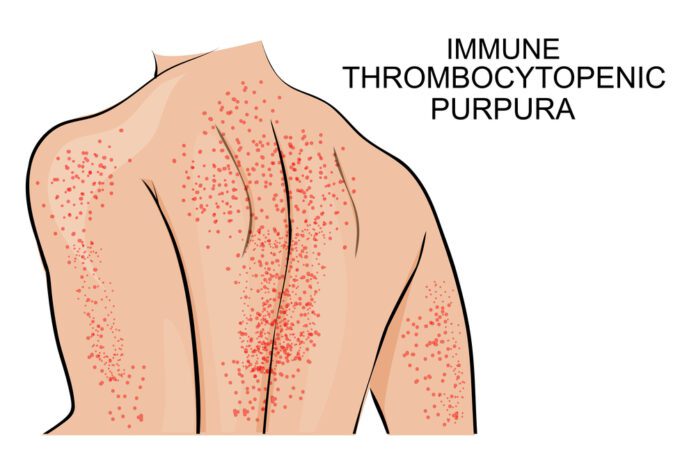
Affected individuals can develop red or purple spots on the skin caused by bleeding just under the skin’s surface. Small spots of bleeding under the skin are called purpura and larger spots are called ecchymoses. People with immune thrombocytopenia can have significant bleeding episodes, such as nose bleeds (epistaxis) or bleeding in the moist lining (mucosae) of the mouth. In severe cases, individuals may have gastrointestinal bleeding or blood in the urine or stool, or heavy and prolonged menstrual bleeding (menorrhagia). In very rare instances, bleeding inside the skull (intracranial hemorrhage) can occur, which can be life-threatening. A greater reduction in platelet numbers is often associated with more frequent bleeding episodes and an increased risk of severe bleeding.
While immune thrombocytopenia can be diagnosed at any age, there are two periods when the condition is most likely to develop: early childhood and late adulthood. In children, the reduction in platelets is often sudden, but platelet levels usually return to normal levels within weeks to months. Immune thrombocytopenia in children is often preceded by a minor infection, such as an upper respiratory infection, but the relationship between the infection and immune thrombocytopenia is not clear. In adults, the development of immune thrombocytopenia is usually gradual and the condition tends to persist throughout life.
Commonly Associated With
ITP; Immune thrombocytopenia; Bleeding disorder – idiopathic thrombocytopenic purpura; Bleeding disorder – ITP; Autoimmune – ITP; Low platelet count – ITP
Causes Of Immune Thrombocytopenic Purpura
ITP occurs when certain immune system cells produce antibodies against platelets. Platelets help your blood clot by clumping together to plug small holes in damaged blood vessels.
The antibodies attach to the platelets. The body destroys the platelets that carry the antibodies.
In children, the disease sometimes follows a viral infection. In adults, it is more often a long-term (chronic) disease and can occur after a viral infection, with the use of certain drugs, during pregnancy, or as part of an immune disorder.
ITP affects women more often than men. It is more common in children than adults. In children, the disease affects boys and girls equally.
The genetic cause of immune thrombocytopenia is unclear. This condition occurs when the body’s own immune system malfunctions and attacks the body’s tissues and organs (autoimmunity). Normally, the immune system produces proteins called antibodies, which attach to specific foreign particles and germs, marking them for destruction. In immune thrombocytopenia, the immune system abnormally destroys platelets and makes fewer platelets than normal. People with immune thrombocytopenia produce antibodies that attack normal platelets. The platelets are destroyed and eliminated from the body, resulting in a shortage of these cells in affected individuals. Some of these antibodies also affect the cells in the bone marrow that produce platelets (known as megakaryocytes), which leads to a decrease in platelet production, further reducing the number of platelets in the blood.
In some people with immune thrombocytopenia, the abnormal immune reactions may coincide with infection by certain viruses or bacteria. Exposure to these foreign invaders may trigger the body to fight the infection, but the immune system also mistakenly attacks platelets.
Genetic variations (polymorphisms) in a few genes have been found in some people with immune thrombocytopenia and may increase the risk of abnormal immune reactions. However, the contribution of these genetic changes to the development of immune thrombocytopenia is unclear.
When the condition is due to the targeted destruction of platelets by the body’s own immune cells, it is known as primary immune thrombocytopenia. Immune thrombocytopenia following bacterial or viral infection is considered primary because the infection triggers a platelet-specific immune reaction, typically without any other signs or symptoms. However, immune thrombocytopenia can be a feature of other immune disorders, such as common variable immune deficiency, which occurs when the immune system has a decreased ability to protect the body against foreign invaders, or other autoimmune disorders such as systemic lupus erythematosus. Immune thrombocytopenia can also occur with other blood disorders, including a form of cancer of the blood-forming tissue known as chronic lymphocytic leukemia, and human immunodeficiency virus (HIV) infection. When immune thrombocytopenia is a feature of other disorders, the condition is known as secondary immune thrombocytopenia.
Symptoms Of Immune Thrombocytopenic Purpura
ITP symptoms can include any of the following:
- Abnormally heavy periods in women
- Bleeding into the skin, often around the shins, causing a skin rash that looks like pinpoint red spots (petechial rash)
- Easy bruising
- Nosebleed or bleeding in the mouth
Exams & Tests
Blood tests will be done to check your platelet count.
A bone marrow aspiration or biopsy may also be done.
Treatment Of Immune Thrombocytopenic Purpura
In children, the disease usually goes away without treatment. Some children may need treatment.
Adults are usually started on a steroid medicine called prednisone or dexamethasone. In some cases, surgery to remove the spleen (splenectomy) is recommended. This increases the platelet count in about half of people. However, other drug treatments are usually recommended instead.
If the disease does not get better with prednisone, other treatments may include:
- Infusions of high-dose gamma globulin (an immune factor)
- Drugs that suppress the immune system
- Anti-RhD therapy for people with certain blood types
- Drugs that stimulate the bone marrow to make more platelets
- People with ITP should not take aspirin, ibuprofen, or warfarin, because these drugs interfere with platelet function or blood clotting, and bleeding may occur.