Overview of Adenomyosis
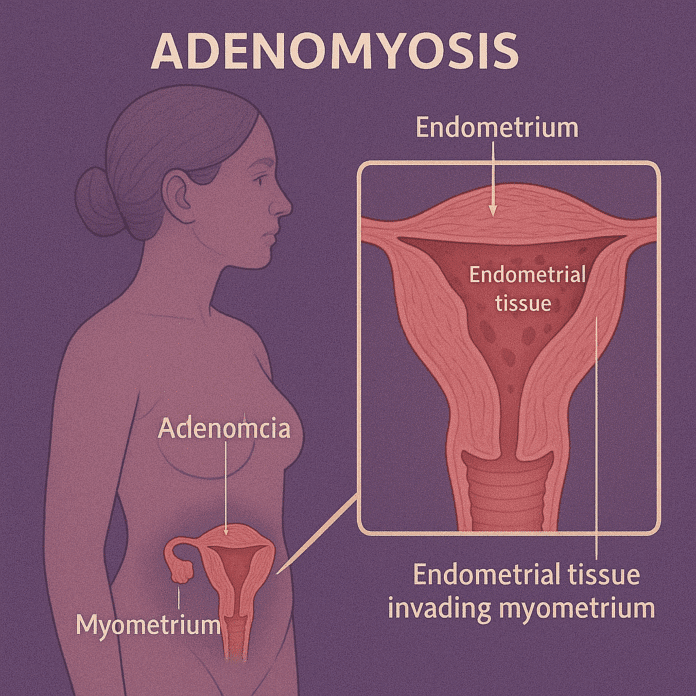
Adenomyosis is a benign gynecological condition in which the endometrial tissue — the lining of the uterus — grows into the myometrium, the muscular wall of the uterus. This misplaced tissue continues to act normally, thickening, breaking down, and bleeding during each menstrual cycle, leading to an enlarged, tender uterus and often heavy, painful periods.
Adenomyosis most commonly affects women between the ages of 35 and 50, especially those who have had multiple pregnancies. While it is not life-threatening, the condition can significantly affect quality of life due to chronic pelvic pain, severe menstrual cramps, and heavy menstrual bleeding. Unlike endometriosis, which occurs outside the uterus, adenomyosis is confined within the uterine wall.
Commonly Associated With Adenomyosis
Several risk factors and conditions are commonly associated with adenomyosis:
- Age: Most common in women aged 35–50 years.
- Parity: More frequent in women who have had multiple pregnancies.
- Uterine surgery: History of cesarean section, dilation and curettage (D&C), or fibroid removal increases risk.
- Hormonal factors: Prolonged estrogen exposure (early menarche, late menopause, or hormone therapy).
- Other uterine conditions: Often coexists with uterine fibroids or endometriosis.
- Genetic predisposition: Family history of adenomyosis or related reproductive disorders.
Causes of Adenomyosis
The exact cause of adenomyosis is not fully understood, but several theories exist regarding how endometrial tissue invades the uterine muscle layer:
- Invasive tissue growth: Endometrial cells may directly invade the uterine muscle after uterine surgery or childbirth.
- Developmental origins: Misplaced endometrial tissue may be present in the uterine wall from birth.
- Inflammation-related disruption: Inflammation of the uterine lining may weaken the boundary between the endometrium and myometrium, allowing tissue to penetrate.
- Hormonal influence: Estrogen plays a key role in stimulating growth of endometrial tissue, and adenomyosis often regresses after menopause when estrogen levels decline.
Symptoms of Adenomyosis
The severity of symptoms varies; some women are asymptomatic, while others experience debilitating menstrual issues. Common signs and symptoms include:
- Heavy or prolonged menstrual bleeding (menorrhagia)
- Severe menstrual cramps (dysmenorrhea) that worsen over time
- Chronic pelvic pain or pressure
- Enlarged, tender uterus (may feel firm or bulky)
- Painful intercourse (dyspareunia)
- Clots or irregular bleeding during menstruation
- Anemia-related symptoms – fatigue, weakness, or dizziness due to blood loss
Symptoms typically improve or resolve after menopause.
Exams & Tests for Adenomyosis
Diagnosis of adenomyosis can be challenging because symptoms overlap with other uterine conditions, such as fibroids and endometriosis. A thorough evaluation includes:
- Pelvic examination: May reveal an enlarged, tender, or boggy uterus.
- Transvaginal ultrasound: Often shows a thickened, heterogeneous myometrium or small myometrial cysts.
- Magnetic resonance imaging (MRI): The most accurate noninvasive tool, revealing thickening of the junctional zone and characteristic uterine changes.
- Endometrial biopsy: Helps rule out cancer or other endometrial diseases but does not confirm adenomyosis.
- Histopathological examination: Definitive diagnosis is often made after hysterectomy when the uterine tissue is examined under a microscope.
Treatment of Adenomyosis
Treatment depends on symptom severity, age, desire for future fertility, and overall health. While there is no permanent cure except hysterectomy, several options can control symptoms and improve quality of life.
1. Medications (Symptom Management):
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Reduce menstrual pain and cramping.
- Hormonal therapies:
- Combined oral contraceptives or progestin-only pills.
- Levonorgestrel-releasing intrauterine device (IUD) to reduce bleeding and pain.
- Gonadotropin-releasing hormone (GnRH) agonists to temporarily suppress menstruation.
2. Minimally Invasive Procedures:
- Uterine artery embolization (UAE): Blocks blood supply to the adenomyotic tissue, reducing symptoms.
- Adenomyomectomy: Surgical removal of adenomyotic tissue while preserving the uterus (option for women wishing to maintain fertility).
3. Definitive Treatment:
- Hysterectomy (removal of the uterus): The only permanent cure, typically reserved for severe cases in women who have completed childbearing.
Lifestyle changes such as regular exercise, stress management, and iron supplementation (for anemia) can further improve outcomes.
Source
- Bergeron C, et al. “Adenomyosis.” Best Pract Res Clin Obstet Gynaecol 2021; 74:36–48.
- Gordts S, et al. “Adenomyosis: a clinical review of a challenging gynecological condition.” Hum Reprod Update 2018; 24(3):305–316.
- National Institute for Health and Care Excellence (NICE). “Heavy menstrual bleeding: assessment and management.” NICE Guideline NG88, 2021.