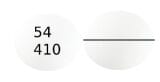
Uses
Levorphanol is used to relieve moderate to severe pain. Levorphanol is in a class of medications called opiate (narcotic) analgesics. It works by changing the way the brain and nervous system respond to pain.
Side Effects Of Levorphanol
Levorphanol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- heartburn
- headache
- stomach pain
- dry mouth
- sweating
- vision problems
- difficulty urinating
Some side effects can be serious. If you experience any of these symptoms or those listed in the Warnings and Precautions sections, call your doctor immediately or get emergency medical treatment:
- nausea, vomiting, loss of appetite, weakness, or dizziness
- agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- inability to get or keep an erection
- irregular menstruation
- decreased sexual desire
- hives
- rash
- itching
- swelling of the eyes, face, mouth, lips, or throat
- hoarseness
- difficulty breathing or swallowing
- changes in heartbeat
Levorphanol may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
Warnings & Precautions
Before taking levorphanol:
- tell your doctor and pharmacist if you are allergic to levorphanol, any other medications, or any of the inactive ingredients in levorphanol tablets. Ask your pharmacist or check the Medication Guide for a list of the inactive ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: antihistamines; buprenorphine (Belbuca, Butrans, in Suboxone, others); butorphanol; medications for cough, cold, or allergies; diuretics (‘water pills’); medications for migraine headaches such as almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex, in Treximet), and zolmitriptan (Zomig); mirtazapine (Remeron); nalbuphine; naloxone (Evzio, Narcan); pentazocine (Talwin); 5HT3 serotonin blockers such as alosetron (Lotronex), dolasetron (Anzemet), granisetron (Kytril), ondansetron (Zofran, Zuplenz), or palonosetron (Aloxi); selective serotonin-reuptake inhibitors such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem, in Symbyax), fluvoxamine (Luvox), paroxetine (Brisdelle, Prozac, Pexeva), and sertraline (Zoloft); serotonin and norepinephrine reuptake inhibitors such as desvenlafaxine (Khedezla, Pristiq), duloxetine (Cymbalta), milnacipran (Savella), and venlafaxine (Effexor); tramadol (Conzip, Ultram, in Ultracet); trazodone (Oleptro); or tricyclic antidepressants (‘mood elevators’) such as amitriptyline, clomipramine (Anafranil), desipramine (Norpramin), doxepin (Silenor), imipramine (Tofranil), nortriptyline (Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil). Also, tell your doctor if you are taking any of the following monoamine oxidase (MAO) inhibitors, or if you have stopped taking them within the past 2 weeks: isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate). Many other medications may also interact with levophanol, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had any of the conditions mentioned in the IMPORTANT WARNING section, a blockage in your stomach or intestines, or paralytic ileus (a condition in which digested food does not move through the intestines). Your doctor may tell you not to take levorphanol.
- tell your doctor if you have or have ever had low blood pressure, seizures, urinary problems, gallbladder problems, or liver, pancreas, kidney, lung, thyroid, or heart disease.
- tell your doctor if you are breastfeeding. If you breastfeed during your treatment with levorphanol, your baby may receive some levorphanol in breast milk. Watch your baby closely for any changes in behavior or breathing, especially when you start taking levorphanol. If your baby develops any of these symptoms, call your baby’s doctor immediately or get emergency medical help: unusual sleepiness, difficulty breastfeeding, difficulty breathing, or limpness. Talk to your baby’s doctor when you are ready to wean your baby. You will need to wean your baby gradually so that your baby will not develop withdrawal symptoms when he or she stops receiving levorphanol in breastmilk.
- you should know that this medication may decrease fertility in men and women. Talk to your doctor about the risks of taking levorphanol.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking levorphanol.
- you should know that levorphanol may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that levorphanol may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up.
- you should know that levorphanol may cause constipation. Talk to your doctor about changing your diet or using other medications to prevent or treat constipation while you are taking levorphanol.
Dosage Of Levorphanol
Levorphanol comes as a tablet to take by mouth. It usually is taken every 6 to 8 hours as needed. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take levorphanol exactly as directed.
Your doctor may start you on a low dose of levorphanol and gradually increase your dose until your pain is controlled. Your doctor may adjust your dose at any time during your treatment if your pain is not controlled. If you feel that your pain is not controlled, call your doctor. Do not change the dose of your medication without talking to your doctor.
Do not stop taking levorphanol without talking to your doctor. Your doctor may decrease your dose gradually. If you suddenly stop taking levorphanol, you may experience withdrawal symptoms such as restlessness; teary eyes; runny nose; yawning; irritability; anxiety; sweating; difficulty falling asleep or staying asleep; chills; back, muscle, or joint pain; nausea; vomiting; loss of appetite; diarrhea; stomach cramps; weakness; fast heartbeat; or fast breathing.
Other
Keep all appointments with your doctor and the laboratory. Your doctor may order certain lab tests to check your body’s response to levorphanol.
Before having any laboratory test (especially those that involve methylene blue), tell your doctor and the laboratory personnel that you are taking levorphanol.
This prescription is not refillable. If you are taking levorphanol to control your pain on a long-term basis, be sure to schedule appointments with your doctor so that you do not run out of medication. If you continue to have pain after you finish your levorphanol prescription, call your doctor.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.