Overview of Acute Lymphoblastic Leukaemia
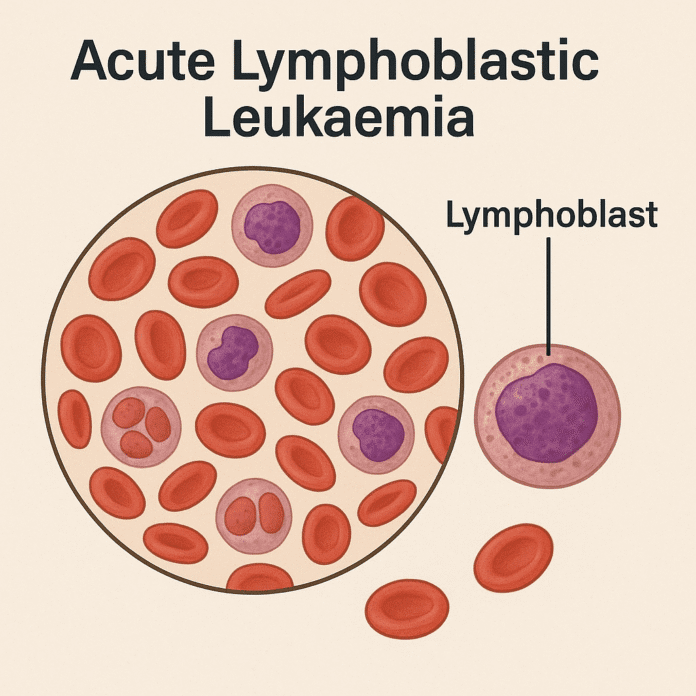
Acute lymphoblastic leukaemia (ALL) is a rapidly progressing cancer of the blood and bone marrow characterized by the uncontrolled proliferation of immature lymphoid cells, known as lymphoblasts. These abnormal cells crowd out normal blood cell production, leading to anemia, infection, and bleeding tendencies. ALL is the most common type of childhood cancer, peaking between ages 2 and 5, but it can also affect adults, where it often has a more aggressive course and poorer prognosis. Prompt diagnosis and treatment are crucial, as ALL can progress quickly if left untreated.
Commonly Associated with Acute Lymphoblastic Leukaemia
ALL is commonly associated with:
- Children under 15 years, though it can occur at any age
- Genetic conditions, such as Down syndrome, Bloom syndrome, and ataxia-telangiectasia
- Previous chemotherapy or radiation therapy, which increases risk
- Family history of leukemia or other hematologic malignancies
- Exposure to high doses of radiation or certain chemicals (e.g., benzene)
- Certain chromosomal abnormalities, such as the Philadelphia chromosome (t[9;22]), which is more common in adult ALL
Causes of Acute Lymphoblastic Leukaemia
The exact cause of ALL is not fully understood, but it is believed to result from genetic mutations in the DNA of bone marrow stem cells that lead to uncontrolled growth of lymphoblasts. Contributing factors include:
- Chromosomal translocations and mutations that activate oncogenes or deactivate tumor suppressor genes
- Genetic predisposition (e.g., inherited syndromes)
- Environmental exposures such as ionizing radiation and certain chemicals
- Previous cancer treatments, which can damage bone marrow DNA
- Random errors during early immune cell development, which can lead to malignant transformation
Symptoms of Acute Lymphoblastic Leukaemia
ALL symptoms typically develop rapidly over weeks due to the bone marrow’s inability to produce healthy blood cells. Common signs and symptoms include:
- Anemia-related symptoms: fatigue, pallor, shortness of breath
- Frequent infections due to low white blood cell count
- Easy bruising or bleeding, nosebleeds, or bleeding gums due to low platelet counts
- Bone and joint pain from bone marrow expansion
- Swollen lymph nodes, liver, or spleen
- Fever and night sweats
- Unexplained weight loss and loss of appetite
- Neurological symptoms (e.g., headaches, vomiting, blurred vision) if the central nervous system is involved
Exams & Tests for Acute Lymphoblastic Leukaemia
Diagnosis of ALL involves a combination of clinical evaluation, blood tests, and bone marrow studies:
- Complete blood count (CBC): Often shows anemia, thrombocytopenia, and abnormal white blood cell counts with circulating lymphoblasts.
- Peripheral blood smear: Reveals immature lymphoblasts.
- Bone marrow aspiration and biopsy: Confirms diagnosis and assesses blast percentage (>20% blasts is diagnostic).
- Immunophenotyping (flow cytometry): Differentiates B-cell from T-cell ALL.
- Cytogenetic and molecular testing: Identifies chromosomal abnormalities (e.g., Philadelphia chromosome) important for prognosis and treatment planning.
- Lumbar puncture: Checks for central nervous system involvement.
- Imaging (e.g., chest X-ray, CT): May detect mediastinal masses, especially in T-cell ALL.
Treatment of Acute Lymphoblastic Leukaemia
Treatment for ALL is intensive and multi-phased, typically involving chemotherapy, targeted therapies, and sometimes stem cell transplantation:
1. Induction Therapy
- Aim: Achieve remission by eradicating leukemic cells.
- Regimen: Combination chemotherapy (e.g., vincristine, corticosteroids, anthracyclines, asparaginase).
2. Consolidation (Intensification) Therapy
- Aim: Eliminate residual disease and prevent relapse.
- Regimen: High-dose chemotherapy ± targeted agents.
3. Maintenance Therapy
- Aim: Prevent relapse over 2–3 years.
- Regimen: Low-dose oral chemotherapy (e.g., methotrexate, mercaptopurine).
4. Central Nervous System (CNS) Prophylaxis
- Intrathecal chemotherapy or cranial irradiation to prevent CNS relapse.
5. Targeted Therapies and Immunotherapy
- Tyrosine kinase inhibitors (e.g., imatinib) for Philadelphia chromosome-positive ALL.
- Monoclonal antibodies (e.g., blinatumomab, inotuzumab ozogamicin) targeting specific leukemic antigens.
- CAR T-cell therapy for relapsed or refractory cases.
6. Stem Cell Transplantation
- Considered in high-risk patients or those with relapsed disease.
With modern treatment protocols, over 85% of children and 40–50% of adults achieve long-term remission.
Source
- Pui C-H, et al. “Acute lymphoblastic leukaemia.” Lancet 2008; 371(9617):1030–1043.
- Terwilliger T, Abdul-Hay M. “Acute lymphoblastic leukemia: a comprehensive review and 2017 update.” Blood Cancer J 2017; 7(6):e577.
- National Cancer Institute. “Childhood Acute Lymphoblastic Leukemia Treatment (PDQ®) – Health Professional Version.” NCI, 2024.