Overview
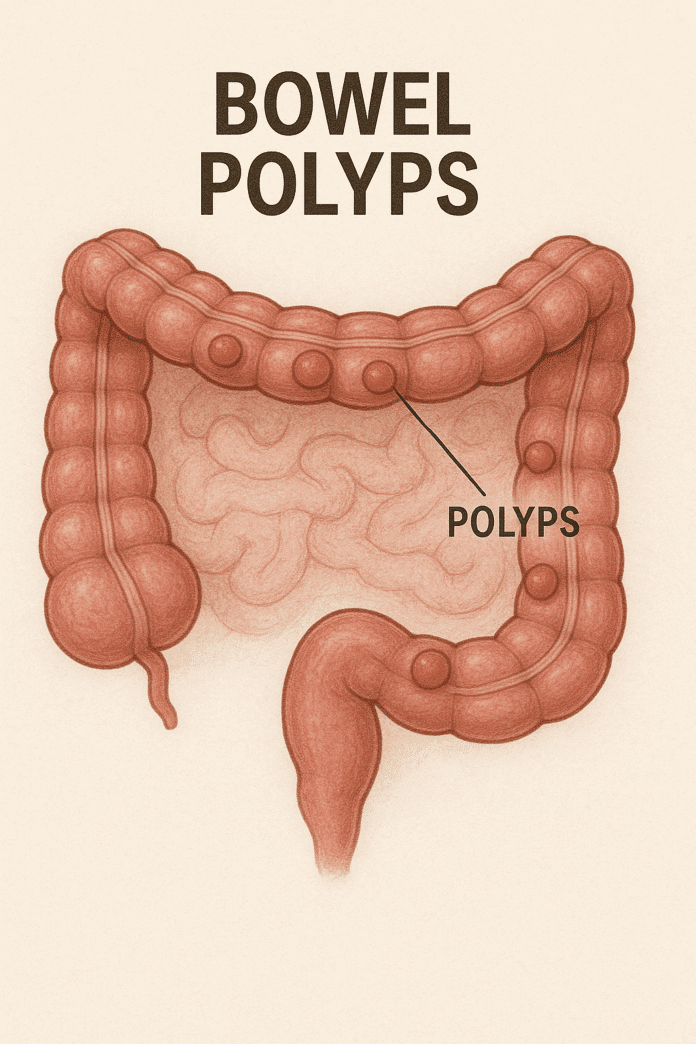
Bowel polyps are abnormal growths that develop on the inner lining of the colon or rectum, parts of the large intestine. Most polyps are benign (non-cancerous), but some can gradually develop into colorectal cancer over time. They vary in size and shape, ranging from small, flat lesions to larger, mushroom-like growths. Bowel polyps are common, especially in people over 50, and often cause no symptoms, making routine screening vital for early detection and removal before they progress to cancer.
Commonly Associated
Other terms and related conditions for bowel polyps include:
- Colorectal polyps
- Colon polyps
- Rectal polyps
- Adenomatous polyps (adenomas)
- Hyperplastic polyps
Causes
The exact cause of bowel polyps is not always known, but several factors increase the risk of their formation:
- Genetic predisposition – Family history of bowel polyps or inherited syndromes such as familial adenomatous polyposis (FAP) and Lynch syndrome.
- Age – Most polyps occur in individuals over 50.
- Dietary factors – High intake of red and processed meats and low fiber intake.
- Lifestyle factors – Sedentary lifestyle, smoking, and heavy alcohol consumption.
- Inflammatory bowel disease – Chronic conditions like Crohn’s disease or ulcerative colitis.
- Obesity and diabetes – Both are linked to a higher risk of polyp formation.
- Cellular changes – Abnormal cell growth in the colon lining can lead to polyp development.
Symptoms
Most bowel polyps do not cause symptoms, especially when small. However, some signs can include:
- Rectal bleeding or blood in the stool
- Mucus in the stool
- Change in bowel habits (diarrhea or constipation) lasting longer than a week
- Abdominal pain or cramping
- Iron-deficiency anemia from slow, chronic blood loss
- Rarely, visible prolapse of a polyp from the rectum
Because polyps are often asymptomatic, regular screening is crucial for early detection.
Exams & Tests
Several diagnostic tools are used to detect and evaluate bowel polyps:
- Colonoscopy – The most effective test, allowing for detection and removal during the same procedure.
- Sigmoidoscopy – Examines the rectum and lower colon for polyps.
- CT colonography (virtual colonoscopy) – A noninvasive scan that visualizes the colon.
- Fecal occult blood test (FOBT) – Detects hidden blood in stool, which may indicate polyps.
- Stool DNA test – Identifies abnormal DNA shed by polyps or cancer cells.
Treatment
The primary treatment for bowel polyps is removal to prevent cancer development:
- Polypectomy during colonoscopy – Most polyps are removed during colonoscopy using a snare or forceps.
- Endoscopic mucosal resection (EMR) – Used for larger or flat polyps.
- Surgical removal – Required for polyps too large for endoscopic removal or if cancer is suspected.
- Regular surveillance colonoscopies – Follow-up screenings are recommended to monitor for recurrence, especially in patients with multiple or high-risk polyps.
Lifestyle changes such as increasing fiber intake, reducing red meat, and quitting smoking can help reduce the risk of new polyp formation.
Source
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Colon Polyps
- American Cancer Society – Colorectal Polyps Overview
- NHS – Bowel Polyps Guide