Overview of Anaphylaxis
Anaphylaxis is a severe, life-threatening allergic reaction that occurs rapidly after exposure to an allergen. It is a medical emergency that can affect multiple organ systems, including the skin, respiratory tract, cardiovascular system, and gastrointestinal tract. Without prompt treatment, anaphylaxis can lead to shock, respiratory failure, or death within minutes.
It is triggered by exposure to substances that cause the immune system to release large amounts of histamine and other mediators, resulting in widespread vasodilation, airway constriction, and tissue swelling. Early recognition and immediate administration of epinephrine are critical for survival.
Commonly Associated with Anaphylaxis
Anaphylaxis can be triggered by a wide range of allergens and is more common in individuals with a history of allergies, asthma, or prior anaphylactic reactions. Common triggers include:
- Foods: Peanuts, tree nuts, shellfish, fish, milk, eggs, soy, wheat.
- Medications: Antibiotics (e.g., penicillin), NSAIDs, chemotherapy drugs, monoclonal antibodies.
- Insect stings: Bees, wasps, hornets, fire ants.
- Latex: Found in gloves, balloons, medical devices.
- Exercise-induced anaphylaxis: Triggered by physical activity, often combined with food intake.
- Idiopathic anaphylaxis: No identifiable cause, though rare.
Risk factors include a history of allergic conditions, asthma, mast cell disorders, and prior episodes of anaphylaxis.
Causes of Anaphylaxis
Anaphylaxis is caused by an overreaction of the immune system to a normally harmless substance (allergen). Upon exposure, immunoglobulin E (IgE) antibodies recognize the allergen and trigger mast cells and basophils to release large amounts of histamine, leukotrienes, prostaglandins, and cytokines.
These mediators cause:
- Vasodilation: Leading to a sudden drop in blood pressure (anaphylactic shock).
- Increased vascular permeability: Resulting in swelling (edema).
- Bronchoconstriction: Narrowing of airways and difficulty breathing.
- Mucous secretion and smooth muscle contraction: Contributing to airway and gastrointestinal symptoms.
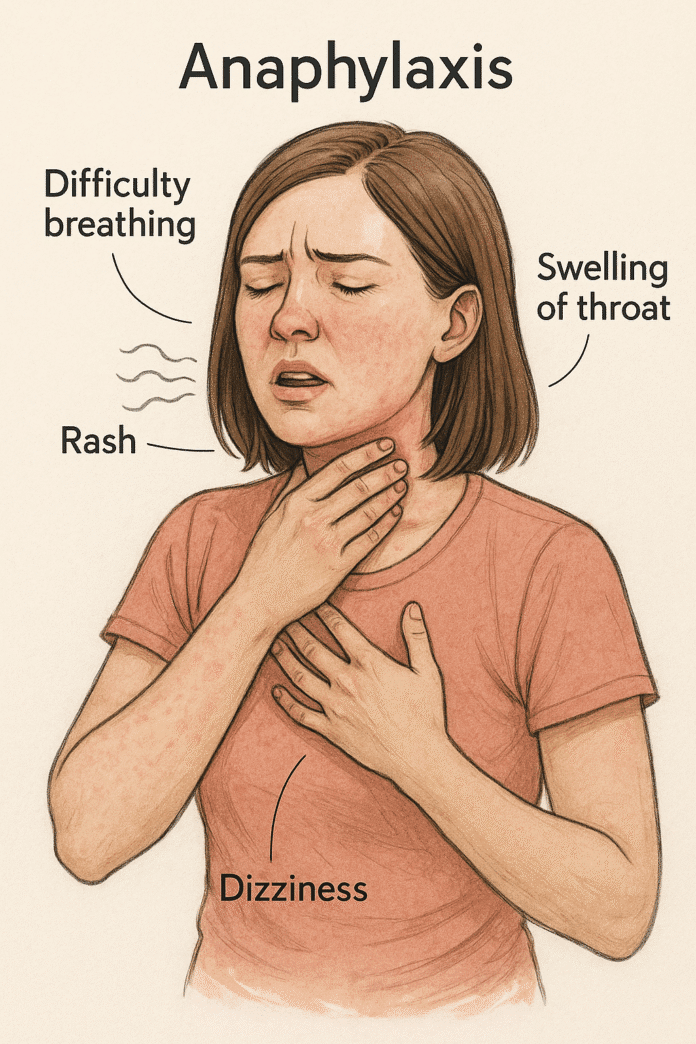
Symptoms of Anaphylaxis
Anaphylaxis usually occurs within minutes of exposure but may develop up to an hour later. It often involves multiple organ systems and progresses rapidly.
Early symptoms:
- Skin flushing, warmth
- Itching, hives (urticaria)
- Swelling of lips, face, eyelids (angioedema)
- Tingling in the mouth or throat
Severe symptoms:
- Respiratory: Shortness of breath, wheezing, throat tightness, hoarseness, difficulty swallowing
- Cardiovascular: Rapid heartbeat, low blood pressure, dizziness, fainting, shock
- Gastrointestinal: Nausea, vomiting, abdominal pain, diarrhea
- Neurological: Confusion, anxiety, sense of impending doom
- Collapse or loss of consciousness in severe cases
Anaphylaxis can be biphasic, with a second wave of symptoms hours after the initial reaction.
Exams & Tests for Anaphylaxis
Anaphylaxis is primarily a clinical diagnosis based on symptoms and history of exposure. Rapid identification is essential, and treatment should not be delayed for testing.
- Clinical criteria: Sudden onset of illness with involvement of skin, mucosal tissue, or both, plus respiratory compromise or reduced blood pressure.
- Vital signs: Hypotension, tachycardia, hypoxia.
- Blood tests (after stabilization):
- Serum tryptase: Elevated levels within 1–3 hours support the diagnosis.
- Allergy testing: Performed later to identify specific triggers (skin prick test, specific IgE test).
Imaging or additional tests are not typically needed during the acute phase.
Treatment of Anaphylaxis
Immediate treatment is critical — delayed intervention increases the risk of fatal outcomes. The cornerstone of therapy is epinephrine, administered as soon as anaphylaxis is suspected.
1. Emergency Management:
- Epinephrine (adrenaline): Intramuscular injection (0.3–0.5 mg in adults; 0.01 mg/kg in children) into the mid-outer thigh. Can be repeated every 5–15 minutes if necessary.
- Call emergency services immediately.
- Positioning: Lay the patient flat with legs elevated unless breathing is difficult (then sit up). Avoid sudden standing.
2. Adjunctive Therapies (After Epinephrine):
- Oxygen therapy: If hypoxic.
- Intravenous fluids: For hypotension or shock.
- Antihistamines (H1 and H2 blockers): Help relieve hives and itching but are not life-saving.
- Corticosteroids: May reduce the risk of biphasic reactions, though evidence is limited.
- Bronchodilators (e.g., salbutamol): For persistent wheezing or bronchospasm.
3. Post-Reaction Care:
- Observation: At least 4–6 hours for mild cases, 12–24 hours for severe cases.
- Referral to an allergist: For identification of triggers and long-term management.
- Epinephrine auto-injector prescription: Patients should always carry one and be trained in its use.
- Emergency action plan: Developed for patients with known severe allergies.
Source
- Simons FE, et al. “World Allergy Organization Guidelines for the Assessment and Management of Anaphylaxis.” World Allergy Organ J 2020; 13(10):100472.
- Shaker M, et al. “Anaphylaxis: Highlights from the Practice Parameter Update 2023.” Ann Allergy Asthma Immunol 2023; 131(5):551–562.
- Lieberman P, et al. “The diagnosis and management of anaphylaxis practice parameter: 2020 update.” J Allergy Clin Immunol 2020; 145(4):1082–1123.