Overview Of Pulmonary Embolism
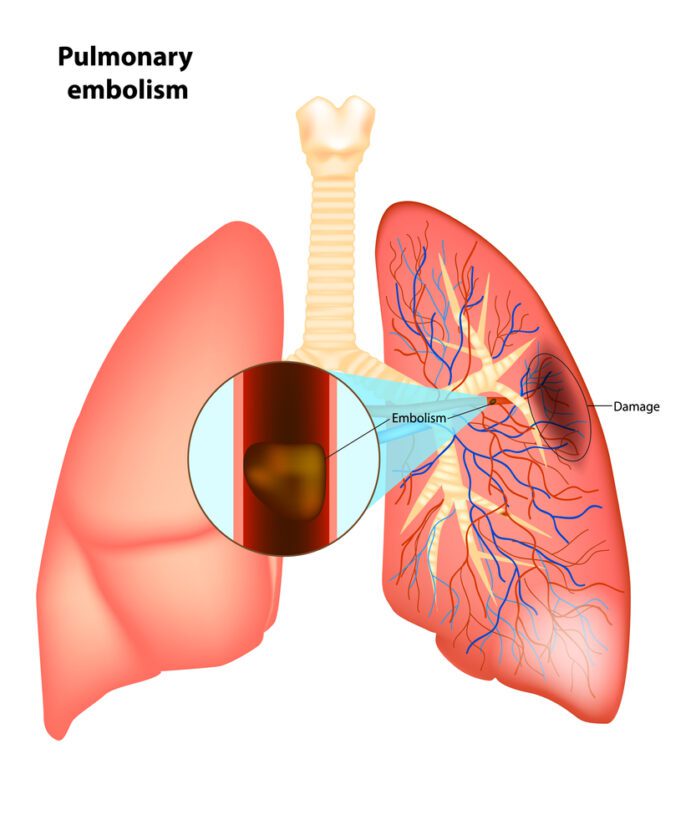
A pulmonary embolism is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.
Commonly Associated With
Venous thromboembolism; Lung blood clot; Blood clot – lung; Embolus; Tumor embolus; Embolism – pulmonary; DVT – pulmonary embolism; Thrombosis – pulmonary embolism; Pulmonary thromboembolism; PE
Causes Of Pulmonary Embolism
A pulmonary embolus is most often caused by a blood clot that develops in a vein outside the lungs. The most common blood clot is one in a deep vein of the thigh or in the pelvis (hip area). This type of clot is called deep vein thrombosis (DVT). The blood clot breaks off and travels to the lungs where it lodges.
Less common causes include air bubbles, fat droplets, amniotic fluid, or clumps of parasites or tumor cells.
You are more likely to get this condition if you or your family has a history of blood clots or certain clotting disorders. A pulmonary embolus may occur:
- After childbirth
- After a heart attack, heart surgery, or stroke
- After severe injuries, burns, or fractures of the hips or thigh bone
- After surgery, most commonly bone, joint, or brain surgery
- During or after a long plane or car ride
- If you have cancer
- If you take birth control pills or estrogen therapy
- Long-term bed rest or staying in one position for a long time
- Disorders that may lead to blood clots include:
- Diseases of the immune system that make it harder for the blood to clot.
- Inherited disorders make the blood more likely to clot. One such disorder is antithrombin III deficiency.
Symptoms Of Pulmonary Embolism
Main symptoms of a pulmonary embolism include chest pain that may be any of the following:
- Under the breastbone or on one side
- Sharp or stabbing
- Burning, aching, or a dull, heavy sensation
- Often gets worse with deep breathing
- You may bend over or hold your chest in response to the pain
Other symptoms may include:
- Dizziness, lightheadedness, or fainting
- Low oxygen level in the blood (hypoxemia)
- Fast breathing or wheezing
- Fast heart rate
- Feeling anxious
- Leg pain, redness, or swelling
- Low blood pressure
- Sudden cough, possibly coughing up blood or bloody mucus
- Shortness of breath that starts suddenly during sleep or on exertion
- Low-grade fever
- Bluish skin (cyanosis) — less common
Exams & Tests
The health care provider will perform a physical exam and ask about your symptoms and medical history.
The following lab tests may be done to see how well your lungs are working:
- Arterial blood gases
- Pulse oximetry
The following imaging tests can help determine where the blood clot is located:
- Chest x-ray
- CT angiogram of the chest
- Pulmonary ventilation/perfusion scan also called a V/Q scan
- CT pulmonary angiogram
Other tests that may be done include:
- Chest CT scan
- D-dimer blood test
- Doppler ultrasound exam of the legs
- Echocardiogram
- ECG
Blood tests may be done to check if you have an increased chance of blood clotting, including:
- Antiphospholipid antibodies
- Genetic testing to look for changes that make you more likely to develop blood clots
- Lupus anticoagulant
- Protein C and protein S levels
Treatment Of Pulmonary Embolism
A pulmonary embolus requires treatment right away. You may need to stay in the hospital:
You will receive medicines to thin the blood and make it less likely your blood will form more clots.
In cases of severe, life-threatening pulmonary embolism, treatment may involve dissolving the clot. This is called thrombolytic therapy. You will receive medicines to dissolve the clot.
Whether or not you need to stay in the hospital, you will likely need to take medicines at home to thin the blood:
- You may be given pills to take or you may need to give yourself injections.
- For some medicines, you will need blood tests to monitor your dosage.
- How long you need to take these medicines depends mostly on the cause and size of your blood clot.
- Your provider will talk to you about the risk of bleeding problems when you take these medicines.
- If you cannot take blood thinners, your provider may suggest surgery to place a device called an inferior vena cava filter (IVC filter). This device is placed in the main vein in your belly. It keeps large clots from traveling into the blood vessels of the lungs. Sometimes, a temporary filter can be placed and removed later.