Overview
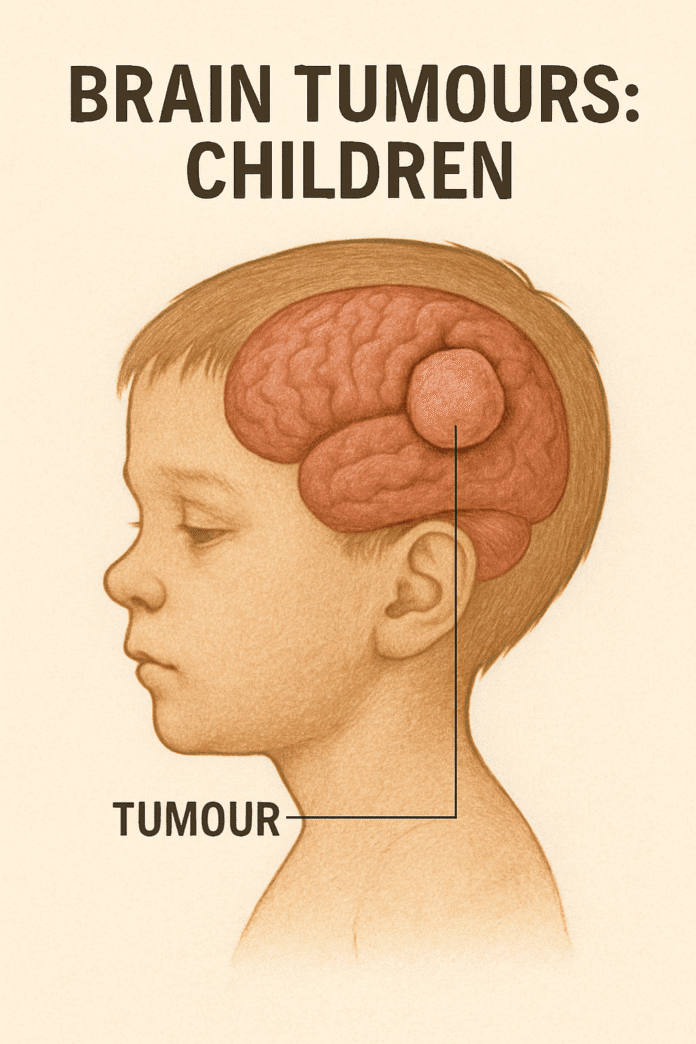
Brain tumours in children are abnormal growths of cells within the brain or central nervous system. They can be benign (non-cancerous) or malignant (cancerous) and are the most common solid tumours in childhood. These tumours can interfere with normal brain function by pressing on surrounding tissues, increasing intracranial pressure, or blocking the flow of cerebrospinal fluid. Early diagnosis and treatment are critical, as outcomes depend on the type, size, and location of the tumour.
Commonly Associated
- Medulloblastoma – the most common malignant brain tumour in children
- Astrocytoma – can range from low-grade (slow-growing) to high-grade (aggressive)
- Ependymoma – develops from ependymal cells lining the ventricles
- Brainstem glioma – occurs in the brainstem, often difficult to treat surgically
- Craniopharyngioma – typically benign but can affect growth and hormone function
Causes
The exact cause is often unknown, but several factors can increase risk:
- Genetic conditions such as Li-Fraumeni syndrome, neurofibromatosis, or tuberous sclerosis
- Inherited mutations that affect tumour suppressor genes
- Radiation exposure, especially previous therapeutic radiation to the head
- Rarely, familial history of childhood cancers
Symptoms
Symptoms depend on tumour size, type, and location but may include:
- Persistent headaches, often worse in the morning
- Nausea and vomiting due to increased intracranial pressure
- Seizures or unusual movements
- Vision changes, double vision, or loss of vision
- Balance and coordination problems
- Behavioral changes or decline in school performance
- In infants: increasing head size or bulging fontanelle
Exams & Tests
Diagnosis involves a combination of neurological evaluation and imaging:
- MRI or CT scan – detailed imaging to locate and assess the tumour
- Biopsy – confirms tumour type and grade
- Lumbar puncture – checks for tumour cells in cerebrospinal fluid (in some cases)
- Blood tests – evaluate overall health and organ function before treatment
Treatment
Treatment depends on the tumour type, location, and child’s age:
- Surgery – often the first step to remove as much tumour as possible
- Radiation therapy – targets residual cancer cells (used cautiously in young children)
- Chemotherapy – may be used alone or alongside other treatments
- Targeted therapy or immunotherapy – newer approaches for specific tumour types
- Rehabilitation – physical, occupational, and cognitive therapy to support recovery
Source
- National Cancer Institute (NCI) – Childhood Brain and Spinal Cord Tumours
- NHS UK – Brain Tumours in Children
- American Cancer Society – Brain and Spinal Cord Tumours in Children