Uses of Dextroamphetamine and Amphetamine
The combination of dextroamphetamine and amphetamine (Adderall, Adderall XR, Mydayis) is used as part of a treatment program to control symptoms of attention deficit hyperactivity disorder (ADHD; more difficulty focusing, controlling actions, and remaining still or quiet than other people who are the same age). Adderall is used to treat ADHD in adults and children 3 years of age and older. Adderall XR is used to treat ADHD in adults and children 6 years of age and older. Mydayis is used to treat ADHD in adults and children 13 years of age and older. Dextroamphetamine and amphetamine (Adderall) are also used to treat narcolepsy (a sleep disorder that causes excessive daytime sleepiness and sudden attacks of sleep) in adults and children 12 years of age and older. The combination of dextroamphetamine and amphetamine is in a class of medications called central nervous system stimulants. It works by changing the amounts of certain natural substances in the brain.
Side Effects of Dextroamphetamine and Amphetamine
Dextroamphetamine and amphetamine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nervousness
- headache
- changes in sex drive or ability
- painful menstrual cramps
- dry mouth
- constipation
- diarrhea
- nausea
- weight loss
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- slow or difficult speech
- dizziness
- weakness or numbness of an arm or leg
- seizures
- motor or verbal tics
- teeth grinding
- depression
- believing things that are not true
- feeling unusually suspicious of others
- hallucinating (seeing things or hearing voices that do not exist)
- agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- mania (frenzied or abnormally excited mood)
- changes in vision or blurred vision
- paleness or blue color of fingers or toes
- pain, numbness, burning or tingling in the hands or feet
- unexplained wounds appearing on fingers or toes
- blistering or peeling skin
- rash
- hives
- itching
- swelling of the eyes, face, tongue, or throat
- difficulty breathing or swallowing
- hoarseness
- Dextroamphetamine and amphetamine may cause sudden death in children and teenagers, especially children or teenagers with heart defects or serious heart problems. This medication also may cause sudden death, heart attack, or stroke in adults, especially adults with heart defects or serious heart problems. Call your doctor right away if you or your child has any signs of heart problems while taking this medication including chest pain, shortness of breath, or fainting. Talk to your doctor about the risks of taking this medication.
Dextroamphetamine and amphetamine may slow children’s growth or weight gain. Your child’s doctor will watch his or her growth carefully. Talk to your child’s doctor if you have concerns about your child’s growth or weight gain while he or she is taking this medication. Talk to your child’s doctor about the risks of giving dextroamphetamine and amphetamine to your child.
Warnings & Precautions
Before taking dextroamphetamine and amphetamine:
- tell your doctor and pharmacist if you are allergic to amphetamine, dextroamphetamine, other stimulant medications such as benzphetamine, lisdexamfetamine (Vyvanse), or methamphetamine (Desoxyn); any other medications, or any of the ingredients in dextroamphetamine and amphetamine preparations. Ask your pharmacist for a list of the ingredients.
- tell your doctor if you are taking the following medications or have stopped taking them in the past 14 days: monoamine oxidase (MAO) inhibitors including isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), or tranylcypromine (Parnate). If you stop taking dextroamphetamine and amphetamine, you should wait at least 14 days before you start to take an MAO inhibitor.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and herbal products you are taking. Be sure to mention any of the following: acetazolamide (Diamox); alpha blockers such as alfuzosin (Uroxatral), doxazosin (Cardura), prazosin (Minipress), tamsulosin (Flomax, in Jalyn), and terazosin; antacids and other medications for heartburn or ulcers such as cimetidine (Tagamet), esomeprazole (Nexium), omeprazole (Prilosec, in Zegerid), and pantoprazole (Protonix); antidepressants (‘mood elevators’); antihistamines (medications for colds and allergies); ascorbic acid (Vitamin C); beta blockers such as atenolol (Tenormin), labetalol (Trandate), metoprolol (Lopressor, Toprol XL), nadolol (Corgard), and propranolol (Inderal, Innopran); buspirone; chlorpromazine; fentanyl (Actiq, Duragesic, Subsys, others); guanethidine (no longer available in U.S.); lithium (Lithobid); meperidine (Demerol); methenamine (Hiprex, Urex); medications for migraine headaches such as almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex, in Treximet), and zolmitriptan (Zomig); quinidine (in Nuedexta); reserpine; ritonavir (Norvir, in Kaletra); certain medications for seizures such as ethosuximide (Zarontin), phenobarbital, and phenytoin (Dilantin, Phenytek); selective serotonin-reuptake inhibitors such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem, in Symbyax), fluvoxamine (Luvox), paroxetine (Brisdelle, Prozac, Pexeva), and sertraline (Zoloft); serotonin and norepinephrine reuptake inhibitors such as desvenlafaxine (Khedezla, Pristiq), duloxetine (Cymbalta), milnacipran (Savella), and venlafaxine (Effexor); sodium bicarbonate (Arm and Hammer Baking Soda, Soda Mint); sodium phosphate; certain thiazide diuretics (‘water pills’); tramadol (Conzip, in Ultracet); or tricyclic antidepressants (‘mood elevators’) such as desipramine (Norpramin) or protriptyline (Vivactil). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking, especially St. John’s wort and tryptophan or nutritional supplements including glutamic acid (L-glutamine).
- tell your doctor if you have glaucoma (increased pressure in the eye that may cause vision loss), hyperthyroidism (a condition in which there is too much thyroid hormone in the body), or feelings of anxiety, tension, or agitation. Your doctor will probably tell you not to take dextroamphetamine and amphetamine.
- tell your doctor if anyone in your family has or has ever had an irregular heartbeat or has died suddenly. Also tell your doctor if you have recently had a heart attack and if you have or have ever had a heart defect, high blood pressure, an irregular heartbeat, hardening of the arteries, heart or blood vessel disease, or other heart problems. Your doctor will examine you to see if your heart and blood vessels are healthy. Your doctor will probably tell you not to take dextroamphetamine and amphetamine if you have a heart condition or if there is a high risk that you may develop a heart condition.
- tell your doctor if you or anyone in your family has or has ever had depression, bipolar disorder (mood that changes from depressed to abnormally excited), or mania (frenzied, abnormally excited mood), motor tics (repeated uncontrollable movements), verbal tics (repetition of sounds or words that is hard to control), or Tourette’s syndrome (a condition characterized by the need to perform repetitive motions or to repeat sounds or words), or has thought about or attempted suicide. Also tell your doctor if you have or have ever had a mental illness, seizures, an abnormal electroencephalogram (EEG; a test that measures electrical activity in the brain), or liver or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking dextroamphetamine and amphetamine, call your doctor. Do not breastfeed while taking dextroamphetamine and amphetamine.
- talk to your doctor about the risks and benefits of taking dextroamphetamine and amphetamine if you are 65 years of age or older. Older adults should not usually take dextroamphetamine and amphetamine because it is not as safe as other medications that can be used to treat the same condition.
- you should know that this medication may make it difficult for you to perform activities that require alertness or physical coordination. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that dextroamphetamine and amphetamine should be used as part of a total treatment program for ADHD, which may include counseling and special education. Make sure to follow all of your doctor’s and/or therapist’s instructions.
- you should know that dextroamphetamine and amphetamine may cause sudden death in children and teenagers, especially children and teenagers who have heart defects or serious heart problems. This medication also may cause sudden death, heart attack, or stroke in adults, especially adults with heart defects or serious heart problems. Call your or your child’s doctor right away and get emergency help, if you or your child has any signs of heart problems while taking this medication including chest pain, shortness of breath, or fainting.
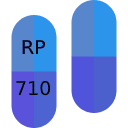
Dosage
The combination of dextroamphetamine and amphetamine comes as an immediate-release tablet (Adderall) and as an extended-release (long-acting) capsule (Adderall XR, Mydayis) to take by mouth. The immediate-release tablet (Adderall) is usually taken 2 to 3 times daily, 4 to 6 hours apart, with or without food. The extended-release capsule (Adderall XR) is usually taken upon awakening with or without food. The extended-release capsule (Mydayis) is usually taken upon awakening and must be taken consistently either with or without food. Dextroamphetamine and amphetamine combination should not be taken in the late afternoon or evening because it may cause difficulty falling asleep or staying asleep. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take dextroamphetamine and amphetamine exactly as directed.
Swallow the extended-release capsules whole; do not chew or crush them. If you are unable to swallow the extended-release capsule, you may open the capsule and sprinkle the entire contents on a teaspoonful of applesauce. Swallow this mixture right away without chewing. Do not store the applesauce and medication mixture for future use, and do not divide the contents of one capsule into more than one dose.
Your doctor will probably start you on a low dose of dextroamphetamine and amphetamine and increase your dose gradually, not more often than once every week.
Your doctor may tell you to stop taking dextroamphetamine and amphetamine from time to time to see if the medication is still needed. Follow these directions carefully.
The medication in each product is absorbed differently by the body, so one dextroamphetamine and amphetamine product cannot be substituted for another product. If you are switching from one product to another, your doctor will prescribe a dose that is best for you.
Other
Keep all your appointments with your doctor and the laboratory. Your doctor may order certain lab tests to check your body’s response to dextroamphetamine and amphetamine.
Before having any laboratory test, tell your doctor and the laboratory personnel that you are taking dextroamphetamine and amphetamine.
This prescription is not refillable. Be sure to schedule appointments with your doctor on a regular basis so that you do not run out of medication.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Source
All information has been provided courtesy of MedLinePlus from the National Library of Medicine and from the FDA.